Introduction
Dementia is a syndrome, chronic or progressive in nature in which there is deterioration in cognitive function it affects memory, thinking, orientation, calculation, learning capacity, language and judgement”.1
The diagnosis of dementia clinically made by Diagnostic and statistical manual of mental disorders.2 The most common type of dementia are Alzheimer's disease, Vascular dementia, Lewy body dementia, Frontotemporal dementia and HIV associated dementia.3
The 3.7 million people are affected by dementia at present in India according to ARDSI and it will double by 2030.4 The estimated cost of dementia care is about 43,000 annually. The challenges posed by dementia on the grounds of health and social issues, unawareness and lack of services due to huge cost for dementia care.4
Lipoproteins are large lipid protein complexes that play a major role in carrier of lipophilic and lipid molecule in plasma and central nervous system.5 The systemic hyperlipidemia may damage the blood brain barrier via inflammatory and other mechanisms, with consequent leakage of serum lipoproteins. Inflammatory cytokines, and other amyloidogenic factors increases oxidative Stress and has important role in attention, cognition.6
The main culprit of Alzheimer's disease is Amyloid-β(Aβ). The increased peripheral lipoproteins, membrane cleavage taking place by b-secreatase and y-secreatase results in amyloidogenic forms that aggregates as extracellular of plaques and Aβ production in Alzheimer's dementia. The increased Cholesterol induces Aβ deposition in the brain and promote production of neurofibrillary tangles (NFT). Aβ induces tau phosphorylation and ROS formation in brain. The peptidyl radical damages mitochondrial DNA, RNA, lipids, protein leads to synapse damage and death of neuronal cell. This is taking place at memory centre and hippocampus of the brain.7
Lipids and lipoproteins were increased in very few studies and associated with dementia at present. The previous studies found decreased levels of lipoproteins in dementia.8 A recent study reported increased levels of lipid and lipoproteins and their association with dementia. Several other studies shows due to increased levels of lipid and lipoproteins may cause neurodegenerative disease. S ome author shows both HDL-cholesterol and total cholesterol can induce the formation of Aβ in invitro studies.11, 10, 9 The Whitehall II Study determined the association between fasting serum lipids and short- term verbal memory in middle-aged adults and found low HDL-cholesterol over a 5-year follow-up period associated with decline memory.12
The present study, we assessed the levels of lipoproteins and their role in Alzheimer's dementia patients and compared with heathy control subject.
Aims and Objective
To evaluate Serum levels of lipoproteins in Alzheimer's dementia.
To find out relationship between lipoproteins levels in Alzheimer's dementia and Control subject.
Subjects and method
The present study was carried out in the department of Biochemistry Grant Medical College and JJ hospital Mumbai. The blood samples was collected and analysed in clinical Biochemistry laboratory. The total duration of study was three months. The patients selected for the present study were attending indoor/outdoor patient department from J J Hospital Mumbai and BRIMS Teaching Hospital Bidar.
The healthy control subjects
50 healthy control subjects in the age group of 70 to 75 years were included in the study. Their physical examination included Systolic blood pressure, Diastolic blood pressure, body mass index, and Mini Mental State score examination was done at our hospital by General Medicine and Psychiatric department. The healthy control subjects shown all tests within normal limit, their MMSE Score was normal (26) and were completely free from psychiatric disorder, addicted to alcohol or intake of any other drug.
The dementia subjects
50 Alzheimer’s type of dementia in the age group of 70 to 75 years were included in the study. Their physical examination included Systolic blood pressure, Diastolic blood pressure, body mass index, and Mini Mental State score examination Score was done at our hospital by General Medicine and Psychiatric department. Physical examination included Systolic blood pressure, Diastolic blood pressure, body mass index were within normal limits except Mini Mental State score examination Score in Alzheimer's dementia subjects. The Alzheimer's dementia was diagnosed by DSM-IV criteria and Mini Mental State examination score. The Mini Mental State score examination less than 12 of patients were selected in our study. This Mini Mental State score examination test administered by senior resident of psychiatric department, which includes questionaries’ related to place, time, attention and calculation, recall, language etc. A score of less than 23 points on the Mini Mental State score examination indicated cognitive impairment.13 The informed written consent was taken from the subjects with the help of subjects family and study was approved by institute ethical committee.
The fasting blood samples was collected from patients and healthy controls with all aseptic precautions in plain polythene tubes for the estimation of lipoproteins. Serum was separated by centrifuging the samples at 3000rpm for 10 minutes and preserved in freezer till the laboratory estimation proceeds.
The Serum Total Cholesterol was estimated by method CHOD-PAP (with LCF) end point. The Serum Triglycerides was estimated by method GPO-Trinder end point. The serum HDL-C was estimated by direct method. LDL-C and VLDL was estimated by calculated using the empirical relation of Friedewald’s (1972). All the kits w ere purchased from ERBA diagnostics Germany (TRANSASIA Biomedicals Ltd) for estimation of lipoproteins. The statistical analysis was carried by Microsoft office 2019 and SPSS software version 18.1- 2017. The Pearson correlations were used as measures of association for the variables. The probability values P < 0.0001 was considered as significant and also data were expressed in mean ± SD form.
Results
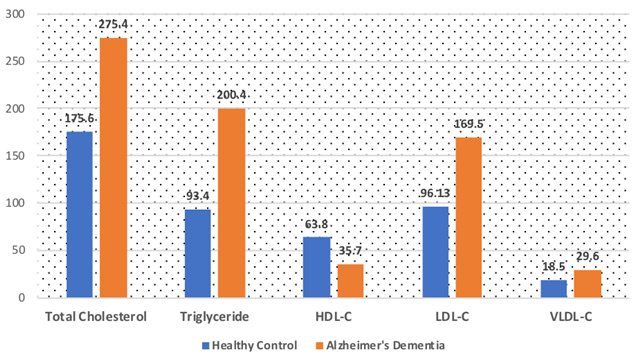
Standard Characteristics of the two groups enrolled in the study are reported in table no-1. No difference appeared in age, systolic, diastolic blood pressure, BMI between Alzheimer's dementia subject and control group. The subjects in Alzheimer's dementia groups had significantly lower MMSE score compare to control group. (P < 0.0001). As presented inTable 2 . Negative correlation was observed but not significant correlation between Total Cholesterol, HDL-C and MMSE in Alzheimer's dementia subjects. In the control group of subject there was lower correlation between Total Cholesterol, Triglyceride, HDL-C, LDL-C and VLDL-C but not statistically significant. The Alzheimer's dementia subjects had statistically significantly higher serum Total Cholesterol, Triglyceride, HDL-C, LDL-C and VLDL-C (P < 0.001) as compared to healthy controls (Table 3). All the subjects in Alzheimer's dementia were male with mean age of cases being 73.42 ± 3.72 and that of controls 74.56 ± 4.30.
Table 1
Standard Characteristics of Alzheimer's Dementia (AD) patients and Control groups.
Table 2
Pearson correlation analysis between Lipoproteins and MMSE score in patients of Alzheimer's Dementia (AD) and Control group
Table 3
The Serum Levels of Lipoproteins in Alzheimer's dementia (AD) and Control group .
All values are expressed as mean ±SD. (* p < 0.001). HDL-C high density lipoprotein cholesterol, LDL-C low density lipoprotein cholesterol, VLDL-C very low density cholesterol.
* p < 0.001 as compared to healthy controls.
Discussion
Lipoproteins are large lipids and protein complexes that play a major role in carrier of lipophilic and lipid molecule in plasma and central nervous system.5 In the central nervous system the functions are performed by neuronal cells of glial cell. Microcytes or microglia having immune related function due to microphage, myelinating cells are oligodendrocytes in the central nervous system and synaptogenesis, neurotransmission by astrocytes. The injury to central nervous system tissue due to reactive mechanism and myelination is separated from specialized cells of barriers called as Blood – Brain barrier.14
Brain cholesterol and lipid homeostasis is largely independent of plasma lipoprotein because the blood brain barrier restricts the transport of these molecules. In the consequence lipoproteins fractions and composition in the central nervous system are different from those in the blood and consists mainly of HDL like particles. Glial cells (in particular astrocytes) the main source of cholesterol and HDL – like particles in the central nervous system.15
The systemic hyperlipidemia may damage the BBB via inflammatory and other mechanisms, with consequent leakage of serum cholesterol, inflammatory cytokines, and other amyloidogenic factors.16 This shown in the Figure 2.16
Figure 1
Role and effect of Increased blood lipoproteins and other factors in Alzheimer's dementia.16
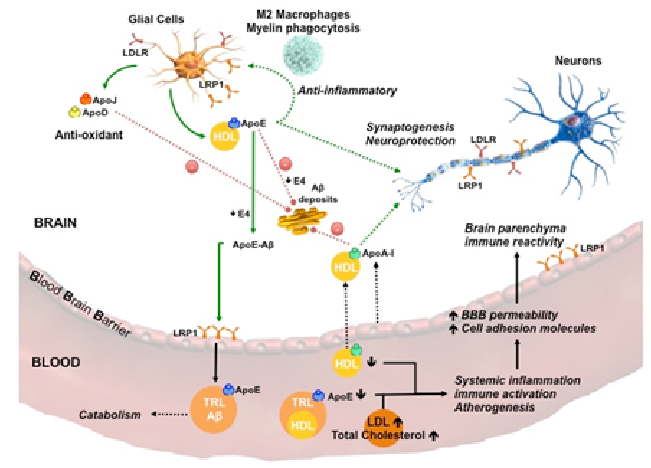
In our study the serum levels of Total cholesterol in Alzheimer’s dementia was significantly increased (P < 0.001) than healthy control subjects (Table 1 Figure 2 Figure 1). Several previous studies found increased midlife cholesterol was associated with Alzheimer's dementia.12 In other studies also shown that Cholesterol in diet increases Aβ deposition in the brain, whereas reduces by cholesterol lowering drugs.18, 17
The several different studies shown that oxidized products of excess cholesterol i.e oxysterols (24-s-hydroxycholetsterol and 27-dehydro-cholesterol) are highly neurotoxic capable passing blood brain barrier leads to neuroinflammation, apoptosis and exocytosis and brain injury, affects on memory centre and progression of Alzheimer's dementia.20, 19
The underlying mechanism is due to increased peripheral Cholesterol, increases Aβ deposition in the brain and promote production of neurofibrillary tangles (NFT). NFT contains hyperphosphorylation tau and Aβ induces tau phosphorylation.21 Our hypothesis shows due to Aβ deposition and reactive oxygen species it damages mitochondrial DNA, RNA, lipids and protein results in to synapse damage, death of neuronal cell. This is taking place at memory centre and hippocampus of the brain.
In our study the serum levels of Triglyceride in Alzheimer’s dementia was significantly increased (P < 0.001) than healthy control subjects (Table 1 Figure 2Figure 1). Several other large studies according to the recent longitudinal cohort study published in neurology, shown increased levels of midlife TG are predictive the presence of Aβ and tau in cognitively healthy individual after 20 years. In this study longitudinal study increased fasting TG levels was associated with increased risk of brain Aβ with tau 20 years later, the se findings were independents of sex, age, APO - E E4.22
The underlying mechanism was due to increased Triglyceride, carries Aβ which effects on Aβ aggregation amyloidogenesis and deposition of Aβ leads to plaque formation.23 Our hypothesis shows due to Aβ induces tau phosphorylation leads and reactive oxygen species formation damages mitochondrial DNA, RNA, lipids and protein results in to synapse damage and death of neuronal cell. This is taking place at memory centre, the hippocampus of the brain
In our study decreased level of serum HDL and increased levels of LDL & VLDL than healthy control subjects (Table 1 Figure 2 Figure 1). The Whitehall II Study determined the association between fasting serum lipids and short- term verbal memory in middle-aged adults and found low HDL-cholesterol over a 5-year follow-up period linked with decline in memory. 12 Several invitro studies show n that increased levels of lipids and lipoproteins may causes neurodegeneration, further both HDL-cholesterol and total cholesterol can induce the formation of Aβ and amyloid plaques.26, 25, 24 Current study supports our study that increased atherogenic lipoproteins such as LDL in systemic circulation of patients of Alzheimer's disease may be intricated in arteriosclerosis, impairment of cerebral blood flow and hypoperfusion in the brain region which promote Alzheimer's disease.27
The underlying mechanism was due to increased inflammatory activity and low-grade systemic inflammation decreases HDL-cholesterol concentration. The inflammatory response is important in neurodegeneration process, HDL-cholesterol diminish a local inflammatory reaction by acting on astrocytes. The inflammatory markers are found in and around in amyloid plaques.29, 28
The another reason was HDL-cholesterol having antioxidant activity, due to decreased levels of HDL-cholesterol and increased LDL-cholesterol results in to oxidized LDL-cholesterol, this oxidized LDL can bind with Aβ and increases Aβ deposition and neurotoxicity in the brain. Aβ aggregation amyloidogenesis and deposition of Aβ leads to plaque formation.30 Our hypothesis shows due to Aβ induces tau phosphorylation and reactive oxygen species formation it damages mitochondrial DNA, RNA, lipids and protein, results in to synapse damage and death of neuronal cell. This is taking place at memory centre, the hippocampus of the brain.
Unfortunately we cannot give any explanation for significantly increased VLDL as there was not single data found in association with the Alzheimer's dementia.
Conclusion
The determination of serum lipoproteins is a routine, not required invasive procedure and cheap method, therefore we suggest that monitoring lipoproteins in older subjects with dementia may be the additional tool to understand basic mechanism of nerve degeneration, memory loss by evaluating lipoprotein levels and their association in Alzheimer's dementia. However further studies are required as serum lipoproteins might be serve potential biomarkers in Alzheimer's disease.
Acknowledgement
The immense help from Authors, scholars whose article are cited and included in references. The publishers, authors, editors also grateful of all those article, journal, books from where the literature has been discussed and reviewed time to time. The authors from Grant medical college Mumbai and BRIMS Bidar for their support and encouragement for carrying out this study.