Introduction
In Chronic kidney disease (CKD), an irreversible deterioration in renal function occurs that classically develops over a period of years. It is defined as abnormalities of renal function and or structure lasting for 3 or more months having several health implications. It eventually lands up in the loss of excretory, metabolic and endocrine functioning of the kidneys. This impaired renal function results in the development of the clinical symptoms and signs which are referred to as uremia. If these subjects are not diagnosed at an early stage and remain untreated without renal replacement therapy, the disease progress to End stage renal failure with poor outcome in terms of morbidity and mortality. Patients with CKD frequently present with signs & symptoms suggestive of thyroid dysfunctions. Previous literature about studies of assessment of functioning of thyroid in CKD patients reports conflicting results. Present study was planned to estimate the thyroid hormones T3, T4 and TSH, Blood urea and Serum Creatinine in cases with CKD and controls.
Materials and Methods
In this case control study which was done from January to June 2015. All diagnosed CKD patients attending Nephrology Department and Dialysis unit in King George hospital, Visakhapatnam were included in the study. The study comprised of 37 diagnosed cases of CKD and 30 healthy age and sex matched controls to evaluate the thyroid hormone profile and renal function tests. The study protocol had been approved by the Institutional Ethics committee and written informed consents were obtained by all participants.
Inclusion criteria
All patients aged 40 to 70 years defined as case of chronic kidney disease by nephrology department were included in the study.
Case of CKD was defined as eGFR ≥ 90 mL/min/1.73m 2 with abnormal urine and blood chemistry, persistent proteinuria or abnormal imaging studies of the kidney or eGFR ≤ 90 mL/min/1.73m 2 The eGFR was done using the 4v-MDRD formula.1
Controls included 30 Healthy age and sex matched subjects aged between 40 -70 years.
Exclusion criteria
Patients with diabetic nephropathy, major diseases like malignancy, cardiovascular diseases were excluded. Patients receiving hormone replacement therapy, corticosteroids, sulphonylureas and phenobarbitones, were not included in the study.
Sample collection
After overnight fast, morning blood samples were collected and allowed to clot. Serum was separated by centrifugation and analyzed for thyroid hormone profile and renal function tests.
Blood urea estimation
Blood urea was estimated by Urease method2 using fully automated Cobas C311 chemistry analyser.
Estimation of Serum Creatinine by Modified Jaffe's method
Creatinine concentration in blood samples were assayed by Jaffe Kinetic method.3
Estimation of T3, T4 & TSH levels by Chemiluminescence immunoassay (CLIA)
Thyroid hormones were estimated using Chemiluminescence immunoassay technique in which principle & procedure for estimation of serum T3 & T4 hormones are similar. This assay is based on a competitive test principle in which polyclonal antibodies are specially directed against T3 T4 and TSH.
Results
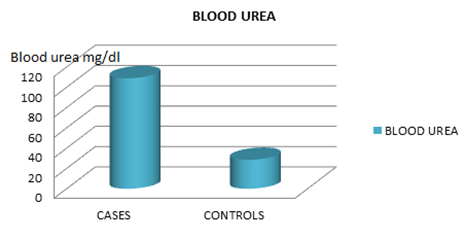
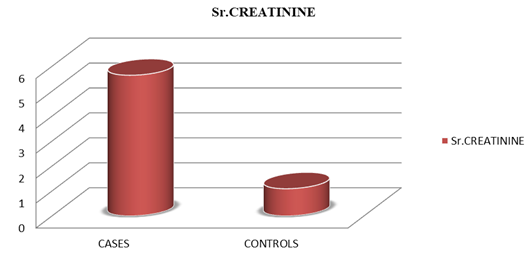
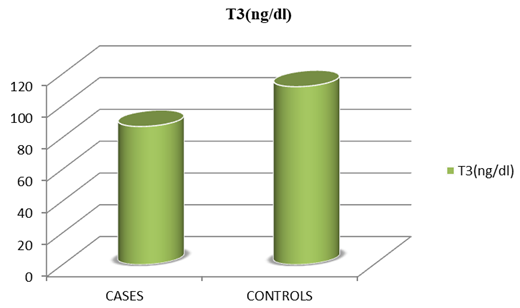
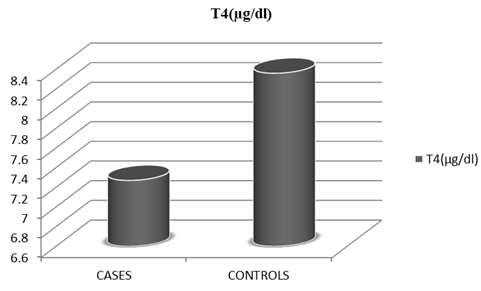
Mean blood urea levels among cases was 108.92 ±52.19 (mg%) and in controls was 28.47±8.40 (mg%) with p value <0.01 which was statistically significant. Mean value of Serum creatinine in cases group was 5.64±2.97 (mg%) and in controls 1.09±0.17 (mg %) and p value was <0.01 which was statistically significant. Mean value of serum T3 concentration among cases group is 86.92±0.23 (ng /dl) and in controls is 111.96±10.17 (ng/dl). It means T3 was decreased in cases as compared to controls with p value <0.01 which was statistically significant. Mean value of T4 among cases was 7.27 (µg/dl) ± 2.19 in comparison to controls 8.36 (µg/dl) ± 0.46 and p value was > 0.01 which was not statistically significant
Mean TSH concentration in cases group was 3.88 (µIU /ml) ± 2.09 which was increased when compared to controls 3.02 (µIU /ml) ±0. 79; P value >0.01 which was not statistically significant.
Among 37 cases, 6 patients (16.2%) have T3, T4 levels below normal range and TSH above the normal range suggestive of hypothyroid state and remaining 31 patients (83.8%) were in euthyroid state. In case group, 27 cases of CKD were managed without dialysis and 10 patients of CKD were on hemodialysis. 3(11%) out of 27 CKD patients without hemodialysis were hypothyroid and 3(30%) out of 10 CKD patients, on hemodialysis were hypothyroid. Thus, we observed decreased levels of T3, T4 increased TSH along with increased serum creatinine levels. The incidence of hypothyroidism was observed to be 16.2% in cases group in comparison to control group.
Table 1
| Age in years | Cases n=37 | Controls n=30 | ||
| Number | Percentage (%) | Number | Percentage (%) | |
| 44-49 | 8 | 21.6 | 7 | 23.3 |
| 50-54 | 11 | 29.7 | 9 | 30.0 |
| 55-59 | 10 | 27 | 10 | 33.3 |
| 60 & above | 8 | 21.6 | 4 | 13.3 |
| Total | 37 | 100.0 | 30 | 100.0 |
Distribution of age (years) of participants between two groups
Table 2
Comparison of studied biochemical parameters in cases and controls (mean ±SD)
Table 3
| T3 (ng /dl) | Cases | Con trols |
| <60 ng/dl | 6(16.2%) | 0 |
| 60- 200 ng/dl | 31(83.8%) | 30(100%) |
| >200 ng/dl | 0 | 0 |
Comparison of serum T3 levels in cases and controls
Discussion
Mean value of T3 in cases was observed to be decreased significantly (p value <0.01) in comparison to controls even though most of them are within the normal range. Presence of altered thyroid hormones profile as either hyperthyroidism or hypothyroidism & euthyroid state have been reported by numerous investigators.8, 7, 6, 5, 4 Consistent low Serum Tri-iodothyronine(T3) levels were observed while serum total and free thyroxine(T4) concentration have been reported as low, normal or high among CKD patients with or without hemodialysis. Serum thyroid stimulating hormone (TSH) levels were reported within normal limits in most of the CKD patients even if with low serum T3 concentration9 One of the possible reasons for altered serum thyroid hormonal levels could be due to the changed binding capacity of serum proteins in CKD due to renal damage. In CKD patients, massive proteinuria occurs that is mainly albuminuria without much changes in Globulin levels. State of Hypothyroidism in CKD is chiefly due to hypoalbuminemia and decreased thyroid binding pre-albumin levels.11, 10 Also raised circulating thyroid binding inhibitors inhibits the binding of thyroid hormones to carrier proteins which may be an additional cause of hypothyroidism in CKD patients.12
Serum TSH levels remain within normal limits in spite of low T3 and T4 concentration. This could not be due to dysfunction in hypothalamo-pitutary axis but because of high TSH response due to hypothyroid state in renal failure patients.12, 9 Few studies reported normal TSH levels due to blunted TSH response to TRH which is suggestive of probability of pituitary dysfunction also.14, 13 Serum thyroid hormone levels depend on the duration of renal failure and its underlying cause. Restoration of normal functioning of kidney resulting in normalization of biochemical parameters of thyroid function with the exception of blunted or absent TSH response to TRH has been reported in patients with CKD after renal transplant. Blunted or absent TSH response to TRH may be a direct consequence of administration of glucocorticoids in these patients. Chronic kidney disease (CKD) patients can be categorized to five stages of kidney damage, from extremely mild stage 1 damage to complete stage 5 kidney failure. In the later stage, the kidneys get contracted. Since last few decades, dramatic increase in the incidence of cases of end stage renal disease has been reported due to altered lifestyle. High prevalence of non-communicable diseases especially Diabetes mellitus and hypertension are responsible for up to two-thirds of cases and other causes include Glomerulonephritis, polycystic kidney disease, malformations, lupus, prostate enlargement. Results of the present study are in accordance with those of previous studies which report decreased levels of T3 in uremia and patients on hemodialysis. 16, 15, 14 Serum total tri-iodothyronine levels were consistently found to be low irrespective of treatment strategy of CKD. Thyroid function studies which were conducted in clinically euthyroid uremic patients demonstrated decrease levels of serum tri-iodothyronine and this reduction in the concentration of T3 has been linked to decrease in peripheral synthesis of T3 from T4. Serum levels of total tri-iodothyronine (T3) in uremic patients is low because source of more than half of the circulating T3 is by peripheral conversion of thyroxine; T4 to T3. Serum T4 levels in cases is apparently decreased compared to the controls, but the difference is not statistically significant. The findings of our study are comparable with those from previous studies. Serum T4 concentration although within the normal range, tend to be lower than in controls are in agreement with the findings of other investigators. The findings of previous studies are conflicting one. Patients with low T3, T4 showed high TSH that suggest maintenance of pituitary thyroid axis. The absence of TSH elevation is generally regarded as an evidence against hypothyroidism state, yet hypothalamo -pituitary dysfunction may also present which can be reflected by the subnormal TSH response to TRH. Thyroid function studies in patients with CKD before & after hemodialysis showed slight increase in T3 concentration without significant change in other thyroid function.19, 18, 17
Among 37 cases; 6 patients (16.2%) we re hypothyroid and remaining 31 patients (83.8%) were euthyroid . Hyperthyroidism was not observed in both groups- cases and controls. All the controls were having euthyroid state. Our study findings are comparable with those of previous studies. CKD is found to be associated with higher prevalence of hypothyroidism, both overt and subclinical, but not with hyperthyroidism. Primary hypothyroidism is mainly in the subclinical form in CKD patients which increases as the glomerular filtration rate (GFR) decreases. The study findings are comparable with the previous study findings that is decreased T3, T4 and increased TSH levels with increased severity of renal damage.22, 21, 20
Conclusion
Serum T3 is decreased in cases group compared to controls and difference is statistically significant whereas T4 and TSH values of cases were not statistically significant when compared with controls. These results points towards the association of low T3 syndrome with CKD. Hyperthyroidism is not observed in both cases & controls groups. TSH increases as T3, T4 decreases suggesting the maintenance of pituitary thyroid axis in this study group. The level of T3, T4 level decreases and TSH increases as severity of renal failure increases (i.e., as serum creatinine increases).