Introduction
Chronic pancreatitis is the inflammation of the pancreas that fails to heal or improve, and worsens over time leading to irreversible damage. It often develops between 30 to 40 years and is more predilected in the male sex. While the major cause of chronic pancreatitis is unknown, the major factors contributing to it are heavy alcohol consumption, genetic mutations, autoimmune conditions and familial history. Pleural effusions occur as a result of both acute and chronic pancreatitis and is usually an indicator of the severity of the disease. Pleural effusion as a consequence of pancreatitis is transient, usually left sided; straw coloured and accounts for 1% of all the cases. Rarely, it may be right sided and haemorrhagic thereby making it difficult to establish the diagnosis, especially if the chest symptoms are disproportionately more than the abdominal symptoms.1 We present a case of bilateral, haemorrhagic pleural effusion secondary to chronic alcoholism induced chronic pancreatitis.
Case History
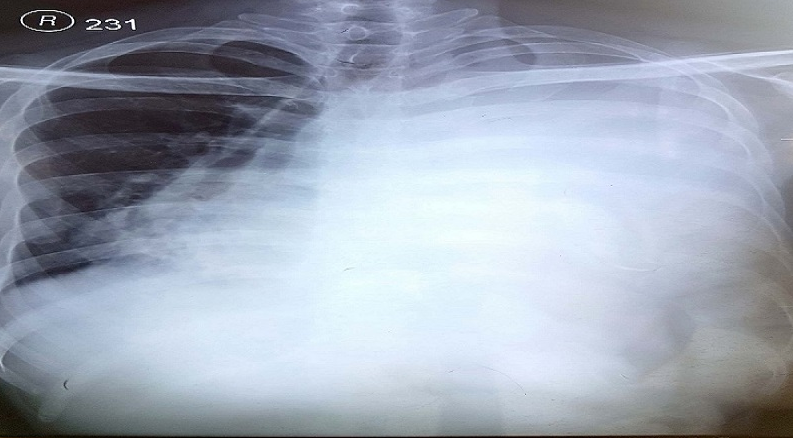
A 38 year old male patient presented with complaints of left sided chest pain and progressive dyspnoea since 40 days. He also complained of intermittent low grade fever, vomiting with reduced appetite, significant weight loss and diffuse abdominal pain over the past 40 days. He gives history of alcohol consumption of 2 to 3 quarters of whiskey per day for the past 9 years. He underwent therapeutic pleural tapping – 5 episodes in other hospitals in view of symptomatic relief. The pulse rate at presentation was 90bpm, blood pressure was 90/56 mmHg and oxygen saturation at room air was 92%. On clinical examination, the trachea was deviated to the right with reduced chest movements, vocal resonance, vocal fremitus and breath sounds on the left, and a dull note on percussion on the left. Chest X ray reveals left sided massive pleural effusion with mediastinal shift to right side (Figure 1). In view respiratory distress, 1000ml of fluid was tapped which was cola colour (Figure 2) and sent for analysis. Pleural fluid amylase was elevated to 12131 U/L. Serum amylase was 6300 U/L.
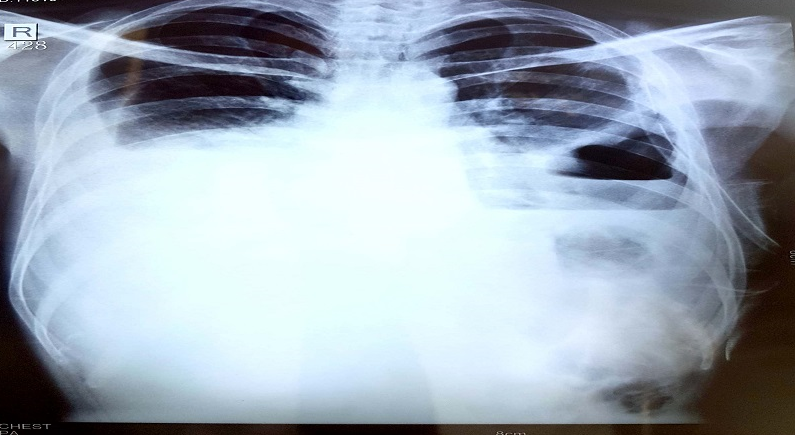
An intercostal drainage tube was placed in the left chest and pleurodesis with 60U of bleomycin was performed in view of multiple septations and thickened pleura. After 1 week of hospital admission patient developed right sided chest pain and Chest X Ray was repeated which revealed Bilateral Pleural Effusion with intercostal drainage tube in situ on left side (Figure 3). Pleural fluid aspiration was done on four occasion at different days for the symptomatic relief. Ultrasound abdomen and computerised tomography of the abdomen revealed the presence of pancreatitis with peripancreatic fistula, pancreatic pseudocysts, dilated pancreatic duct and spillage in the paracolic gutter. Upper gastrointestinal endoscopy showed linear erosions at the lower end of Oesophagus. Endoscopic Retrograde Cholangio Pancreatography (ERCP) showed the presence of a stricture in the proximal pancreatic duct with leak in the distal part of pancreas. A tapered 7 french stent was placed in the pancreatic duct across the leak. Patients symptoms began to resolve over a period of 2 weeks. On follow up after eight weeks patient was symptomatically better with evidence of resolution of pleural effusion on Chest X ray (Figure 4).
Discussion
Chronic pancreatitis is persistent, progressive and permanent damage of the pancreas due to long standing inflammation. It may be of the chronic relapsing or the chronic persistent varieties. The chronic persistent variety usually develops complications like calcifications in the duct of the parenchyma. Histopathological features of chronic pancreatitis include focal necrosis, segmental, sometimes diffuse fibrosis, parenchymal calcification, ductal calculi and stricture or dilation of the pancreatic duct. The classical triad of chronic pancreatitis – pancreatic calcification, steatorrhea and diabetes is present in one third of the patients. The primary investigating modalities for chronic pancreatitis include the CT scan of the abdomen which holds 95% specificity and 90% sensitivity and shows the presence of pancreatic pseudocysts, calcifications, ductal stones, strictures and dilations, vasculature, fibrosis and involvement of the surrounding structures. The ERCP is useful in chronic pancreatitis in mainly identif ying the structural defects in the pancreas including the altered ductal anatomy. The major complications developing as a consequence of chronic pancreatitis include pseudocyst of pancreas, pancreatic ascites, pancreatic pleural effusion, common bile duct stricture due to oedema or inflammation, peptic ulcer, carcinoma pancreas, pancreatic fistulas.
The pleural cavity lies between the lungs and the precordia l wall and usually consists of a very thin layer of fluid called the pleural fluid, which serves as a friction system in the cavity. Pleural effusion is when there is an excess quantity of pleural fluid in the pleural cavity. Typically, fluid enters the pleural cavity from the parietal pleura capillaries and is removed via the parietal pleura lymphatics. A pleural effusion develops when there is increased pleural fluid formation (from the interstitial spaces, the parietal pleura, or the peritoneum) - transudative effusion or when there is reduced fluid removal by the lymphatics - exudative effusion.
Causes of pleural effusion with high amylase are usually acute or chronic pancreatitis with pseudocyst or pancreaticopleural fistula, oesophageal perforation and some neoplastic diseases like adenocarcinoma of lung, lymphoma, ovarian, rectal, cervical, breast and pancreatic cancers.1 Fluid accumulation within the abdominal and the lung spaces are rare complications of both chronic and acute pancreatitis, and are associated with a mortality rate of about 20% to 30%. Pleural effusions in pancreatitis are mostly small, occasionally bloody, and typically have high amylase (up to 30 times more than normal serum value) and protein(> 30 gm/L). Most of the pleural effusions are left-sided (68%), followed by right sided (20%) and bilateral (15%).2 Two important causes of pleural effusion are transdiaphragmatic blockade of lymphatics or pancreaticopleural fistulae occurring secondary to leak and alteration of the pancreatic duct or pseudocyst formation caused by an episode of acute pancreatitis. The pancreatic enzymes can leak up into the mediastinum and then rupture into the pleural space either on left side or bilaterally and hence a connection is formed between the pancreatic duct and the pleural cavity. Close to one third of all patients with an internal pancreatic fistula have pleural effusion.