Introduction
A viral infection spread by mosquitoes known as dengue is recognized for having extremely high rates of mortality and morbidity. The main carriers of this viral illness are mosquitoes. Around 2.5 billion people around the world are infected with the virus.1 Although it is an old disease, dengue fever (DF) was first identified and recorded in Batavia in 1779. A year later, Philadelphia, USA, declared it to be a pandemic.2 Several species of female Aedes mosquitoes carry the dengue virus, which is transmitted by Aedes aegypti. After three to fifteen days of infection, the person may experience a very high fever as well as other side effects like headache, fever, rashes, renal failure, thrombocytopenia, etc. The infection begins with a slight fever.3 The presence of viraemia can be detected within 24-48 hours prior to the commencement of a fever, which lasts for 5-6 days. Infected patient blood, serum, and plasma as well as tissues from fatal cases can all be found to contain the infective virus, its particular RNA, and the NS1 protein.4 According to the stage of infection, different diagnostic tests will be relevant such as RT-PCR, ELISA, for the detection of viraemia, non-structural 1 (NS1) antigen, and antibodies that fluctuate with time.5 Future directions for preventing and treating dengue fever include the control of mosquito (vector) transmission, the creation of a dengue vaccine, and the development of antiviral medications. Guppies (Poecilia reticulata) or copepods (Doridicola agilis) can be kept in standing water to control mosquito (vector) transmission, and the mosquito population can be infected with bacteria from the Wolbachia genus.6
History
There is currently no proof indicating when the dengue virus was originally identified in humans. Although it is an old disease, dengue fever (DF) was first identified and recorded in Batavia in 1779. A year later, Philadelphia, USA, declared it to be a pandemic.2 According to WHO, 1.2 million persons contracted the DF in 1998. Then, 30 times more infections were reported 50 years later. A medical encyclopedia reported another incidence in China in 1992. In the 18th and 19th centuries, as global trade increased, port cities urbanized, making them the perfect places for the spread of the mosquito vector, Aedes aegypti.2, 7
When the first dengue pandemic struck concurrently in Africa, Asia, and North America, it shocked the world.8 Currently, it appears from the available information that there are about 50 million instances of DF in a hundred different countries around the world.9 When an infected Aedes mosquito species (Ae. aegypti or Ae. albopictus) bites a human host, DENV is spread between individuals.7 The West Nile viruses can also be carried by these insects. A change in ecology caused an epidemic of dengue hemorrhagic fever (DHF) in Southeast Asia.10 Plasma leakage, hypovolemia, an increase in vascular permeability and shock are some of its symptoms of dengue fever. About 4.2 million cases of the dengue virus were reported by WHO in 2019.11
Etiology & Epidemiology
Agent: A Flaviviridae family member, the dengue virus. DENV-1, DENV-2, DENV-3, and DENV-4 are the four viral serotypes. Dengue serotypes secondary infections, or numerous infections with various serotypes, are that produce the severe form of the disease are also known as DHF or DSS.12
Vector: The two primary dengue pathogens are "Aedes aegypti" and "Aedes albopictus." It is a little, black mosquito, about 5 mm in length, with white stripes called "tiger mosquito”. The virus must grow within its own body for seven to eight days in order to propagate the sickness. They both have a high vector graphics competency for the dengue virus, which means they are both very susceptible to infection, capable of reproducing the virus, and able to spread the virus to new hosts. The Aedes aegypti mosquito is the main carrier of DENV. It breeds primarily in artificial containers and lives in urban areas. The daytime feeder, Aedes aegypti, is most active in the early morning and just before dusks each evening.13
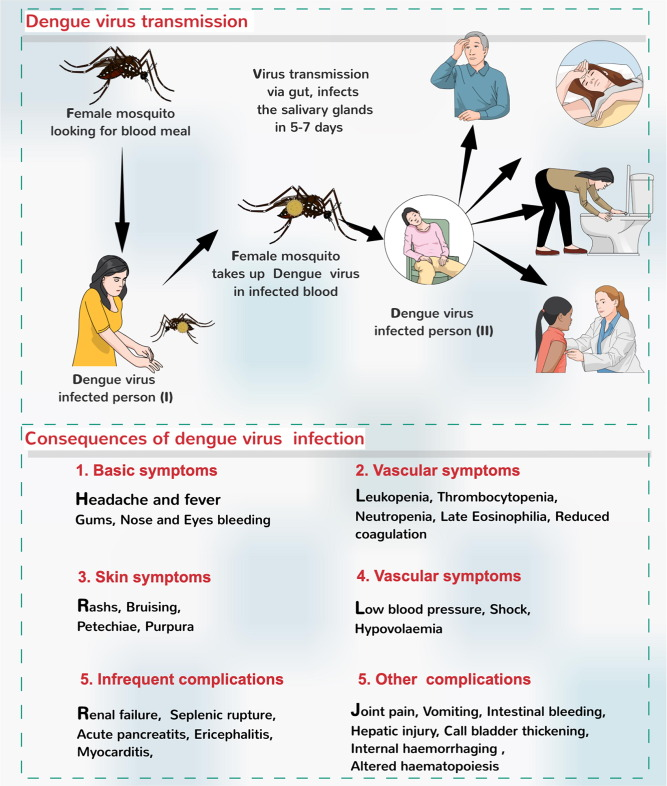
Dengue Transmission
Mosquito-to-human transmission
The virus spreads to humans through bites from infected female mosquitoes, primarily the Aedes aegypti mosquito. After ingesting the DENV-infected person, the mosquito feeds on the virus, which then multiplies in the mosquito's midgut before migrating to secondary tissues like the salivary glands. The extrinsic incubation period (EIP) refers to the interval between swallowing the virus and passing it on to a new host. An EIP of 8–10 days is required for an insect to become pathogenic and susceptible to spread the disease.14
Human-to-Mosquito transmission
Mosquitoes can pick up the DENV virus from people who have it. This can include those who have symptomatic dengue disease, those who are pre-symptomatic (have not yet developed symptoms), and those who show no signs or symptoms of sickness (they are asymptomatic).14
Other modes of the transmission
The main way that the dengue virus spreads between people is through mosquito vectors. However, there is evidence that maternal transfer may occur (from the pregnant mother to the baby). Although the risk of vertical transmission appears to be modest, it appears to be linked to the time of the dengue infection during pregnancy.14, 15
Epidemic dengue and hyperendemic dengue are the two main ways that dengue is transmitted. Epidemic dengue is the term used when a single strain of DENV causes infection and transmission. Epidemics of dengue were more frequent before World War II. All age groups are impacted by an epidemic; however, DHF is a rare occurrence. The co-circulation of several DENV serotypes in a community is referred to as hyperendemicity. The rise of hyperendemicity in a region is associated with recurring epidemics.16
Clinical Features
The dengue fever, also known as "break-bone fever" refers to the accompanying joint and muscle difficulties and often characterized by a fast onset of fever, headache (often behind the eyes). The three stages of the infection's progression are feverish, critical, and recovery. The febrile phase, which typically lasts 2–7 days, is characterized by high fevers, frequently exceeding 40°C (104°F), along with generalized pain and a headache. At this stage, flushed skin and a few petechiae, little red spots caused by ruptured capillaries, may appear. If there is a critical phase, it usually lasts one to two days and comes after the high fever has subsided. Due to increased capillary permeability and leakage, there may be substantial fluid collection in the chest and abdominal cavity during this period. This causes the organs and circulation to become depleted of fluid. Organ malfunction and significant bleeding (mostly from the gastrointestinal system) are possible during this phase. Less than 5% of dengue cases result in shock and bleeding, but those who have had a prior infection with another serotype of the virus (referred to as a "secondary infection") are more likely to experience these complications. The absorption of the fluid that escaped into the bloodstream starts the recovery phase. This often takes place over the course of 2-3 days. Although there may be intense itching and a fever, the improvement is frequently startling. A fluid overflow situation may develop during this period, and if it impacts the brain, it could cause seizures or a reduction in consciousness.17
Laboratory Diagnosis
The finding of viremia DENV viremia can be identified 24–48 hours before the development of fever and lasts for 5–6 days. Infected patient blood, serum, and plasma as well as tissues from fatal cases can all be found to contain the infective virus, its particular RNA, and the NS1 protein during this time.4 For epidemiological monitoring and clinical diagnosis, DENV infection is confirmed using virological, molecular, and serological techniques. Anti-IgM antibodies can be found in samples taken on day 6 of acute symptoms, which can serve as a presumptive diagnosis for patients who are thought to have dengue. Commercially accessible kits are available for ELISA and less sensitive fast test formats for IgM or IgG detection.18 The main microbiological techniques include virus segregation in cell cultures, nucleic acid demonstration by polymerase chain reaction (PCR), and serological detection of viral antigens (like NS1) or specific antibodies.19
Hemotological changes
The first alterations in laboratory tests are a drop in white blood cells (leukopenia), followed by a decrease in platelet count (thrombocytopenia).16
Biochemical changes
Dengue fever is characterized by various biochemical attentions such as significant increase in the levels of serum transaminases (viz., AST, ALT & ALP), raised serum bilirubin level, and significantly decreased serum calcium level.20, 21, 22, 23, 24 Furthermore, a pilot study conducted in Mexico & other places demonstrated that oral CaCO3 plus vitamin D3 supplementation significantly increased the platelets & improved the overall clinical condition and reduced the duration of illness.25, 26, 27
Virus detection
The most conclusive proof of infection is the isolation of dengue virus or the identification of dengue viral RNA or protein in an acute phase serum or tissue material. In general, virus isolation and RT-PCR (reverse transcriptase-polymerase chain reaction) should only be done when absolutely necessary for epidemiologic reasons or as part of clinical research studies. The ideal specimens for virus isolation are serum or plasma, though occasionally liver tissues can also be used once the virus has been removed from the serum. Regardless of the specific technique employed, the best detection results from specimens collected during the feverish episode, soon after the onset of symptoms. In terms of sensitivity to viral isolation, RT-PCR is equivalent. The only technique that can identify viruses in a clinically useful amount of time is RT-PCR, despite being technically challenging and not being frequently used (one to two days).17, 28
Treatment
Patients with dengue fever should be advised to continue consuming oral fluids in order to prevent dehydration. Acetaminophen can be used as needed to treat myalgia and fever. Aspirin and other non-steroidal anti-inflammatory drugs should generally be avoided due to the possibility for bleeding problems and Reye's syndrome in children. The most crucial step in treating a dengue fever patient is to thoroughly assess them for potential complications, like early signs of DHF (severe menorrhagia or gastrointestinal bleeding that necessitates blood transfusion). Rarely administered, platelet transfusions may be necessary in individuals with severe thrombocytopenia (10,000/mm3) and ongoing bleeding.11, 16, 29
Dengue hemorrhagic fever
To avoid or treat hypovolemic shock, it's crucial to aggressively replace intravascular volume when there is plasma leakage in DHF. Oral rehydration may be sufficient in moderate cases, especially when medical treatment is sought promptly. However, intravenous fluid therapy is advised for patients who have a history of intravascular fluid loss. In individuals who have substantial bleeding, blood transfusions are necessary.4
Treatment of shock
As per WHO regimen, an intravenous fluid therapy is necessary for patients who are in shock. A rapid initial bolus of 5 percent dextrose in normal saline or Ringer's lactate is advised. It should be followed by a continuous infusion of the medication (10 to 20 mL/kg per hour) until the patient's vital signs and urine output return to normal. After then, the infusion rate can be gradually decreased until it equals plasma fluid losses.11, 16
Prevention
Personal prophylactic measures including bed nets when in bed (even during the day), using insecticide-treated materials (ITMs) such as; window curtains, applying mosquito repellent creams (including DEET, IR3535, or Icaridin), coils, and making it a habit to wear full-sleeve shirts and trousers.30
Biological control
Fish: Open freshwater wells and big water tanks are examples of confined water sources where viviparous species of Poecilia reticulata have been utilized. Use only locally adapted larvicidal fishes.
Predatory Copepods: Only some container habitats have shown these tiny freshwater crustaceans to be effective.
Endosymbiotic control: Wolbachia (an intracellular parasite)-infected mosquitoes are less likely to contract DENV than the wild type Aedes aegypti mosquito.
Larvicidal use in large breeding containers; insecticide spray: Space sprays can be used as thermal fogs and cold aerosols.
Chemical Control Formulations made of oil are recommended because they prevent evaporation. Organophosphorus compounds (such as fenitrothion and malathion) and pyrethroids are a couple of the regularly used insecticides (bioresmethrin, cypermethrin).
Environmental Controls: Locating pest breeding grounds and getting rid of them; maintaining roofs and sunshades; covering buckets and other containers used to store water properly.11, 16, 29
Health education
The most effective tool in the war against dengue is health education. For the dengue management programme to be implemented effectively, detailed public education about dengue is required. Mass awareness campaigns or audiovisual media can be used to sensitize the public. Sensitization of the community is necessary to ensure their active participation in dengue control initiatives.29
Vaccination
The first licenced live recombinant tetravalent dengue vaccine, CYD-TDV, has been given the go-ahead for endemic locations in 20 different nations. There are currently four different serotypes of tetravalent vaccinations being developed. One tetravalent live attenuated dengue virus vaccine showed 100%, 100%, 90%, and 70% seroconversion rates against dengue serotypes 1, 2, 3, and 4. Additionally, challenges with the other dengue serotypes revealed protection in 50 to 80% of animals compared to controls, providing complete protection against viremia from inoculation with serotype 2. Travelers are advised to: Due to their lack of prior exposure to dengue viruses, the majority of travelers from non-endemic countries have a very low risk of developing DHF. The main method of preventing dengue virus infections in tourists is avoiding contact with infected A. aegypti mosquitoes. Most of these mosquitoes reside in and around homes in metropolitan settings.29, 31
Conclusion
Many individuals have died from dengue virus over the world, and the majority of the rising instances have been connected to urbanization. The doctor should be knowledgeable about the many clinical manifestations of this illness and ensure that a prompt, effective treatment plan is in place. The most sensible suggestion, however, is to continue and improve current dengue prevention measures, particularly during the ongoing COVID-19 outbreak. Future strategies to combat this terrible illness focus on mosquito control techniques, vaccine research, and antiviral medication regimen.