- Visibility 211 Views
- Downloads 21 Downloads
- DOI 10.18231/j.ijcbr.2024.022
-
CrossMark
- Citation
Bone health in crisis: Addressing Vitamin D deficiency in orthopedic practice
Introduction
Vitamin D plays a crucial role in calcium and phosphorus metabolism, which are essential for healthy bone formation and musculoskeletal development in children. With its deficiency, children are at risk for several musculoskeletal conditions due to reduced bone mineral density (BMD). Despite the abundant availability of sunlight, vitamin D deficiency remains highly prevalent among children worldwide, including regions with abundant sunshine. Sedentary lifestyles, inadequate outdoor activity, and poor dietary intake further exacerbate the issue. This review focuses on the orthopedic implications of vitamin D deficiency in children and explores how modern lifestyle factors contribute to this growing health concern.[1]
Vitamin D deficiency has been historically linked to various musculoskeletal conditions, with rickets being one of the earliest recognized disorders. In the 17th century, rickets was prevalent among children in industrialized cities with limited sunlight exposure. [2] The discovery of vitamin D in the early 20th century led to fortification of foods, significantly reducing rickets in many countries.
However, vitamin D deficiency remains a global public health issue, especially in children, due to modern lifestyles. Reduced outdoor activity, excessive screen time, urbanization, and the use of sunscreen have contributed to insufficient sun exposure. This has resulted in a resurgence of conditions such as rickets, osteomalacia, and an increased incidence of fractures, growth retardation, and muscle weakness in children.
Prevalence is particularly high in regions with limited sunlight or where cultural practices limit skin exposure. Studies show that vitamin D deficiency affects 30-50% of children globally, making musculoskeletal complications a significant concern in pediatric health. The prevalence of vitamin D deficiency in children varies significantly across different countries due to factors such as geographic location, lifestyle, diet, and cultural practices ([Table 1])
Literature Review
Vitamin D physiology and musculoskeletal health
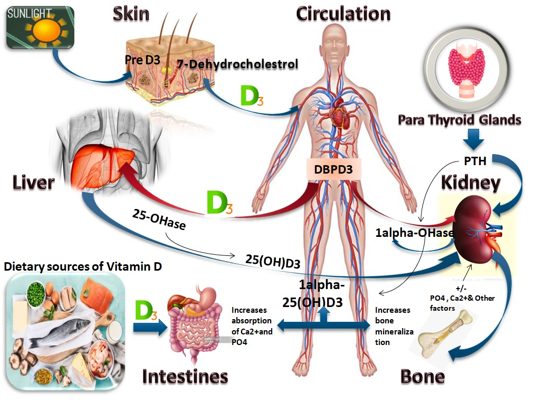
Vitamin D, synthesized in the skin via exposure to ultraviolet B (UVB) rays, undergoes conversion to its active form, calcitriol, in the liver and kidneys. Calcitriol enhances intestinal absorption of calcium and phosphorus, critical for bone mineralization. In children, deficient levels of vitamin D can lead to impaired bone growth and structural integrity, causing a spectrum of orthopedic disorders.[3] ([Figure 1])
Orthopedic Conditions Associated with Vitamin D Deficiency
Vitamin D deficiency in children has profound orthopedic implications, most notably seen in conditions like rickets, osteomalacia, increased fracture risk, and impaired skeletal development. Rickets is the classic manifestation of severe vitamin D deficiency, characterized by defective bone mineralization and growth plate abnormalities, leading to clinical presentations such as bowing of the legs (genu varum), delayed fontanelle closure, and skeletal deformities. Osteomalacia, prevalent in older children and adolescents, results in soft bones due to defective mineralization, manifesting as musculoskeletal pain, skeletal deformities, and heightened fracture risk. Vitamin D deficiency is also strongly associated with fractures, as it reduces bone mineral density (BMD), making children more susceptible to fractures, particularly in the forearm and lower extremities, even from low-energy impacts. Additionally, vitamin D is critical for optimal skeletal development and growth, especially during childhood’s peak bone mass acquisition period. Inadequate vitamin D levels during this time can lead to stunted growth, increasing the long-term risk of osteoporosis and other musculoskeletal disorders. Understanding these conditions underscores the vital role of vitamin D in orthopedic health and emphasizes the need for early prevention and intervention.[4], [5] ([Table 2])
The importance of this literature on the role of vitamin D deficiency in musculoskeletal conditions is multi-faceted: ([Table 3]) [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24]
Enhanced Understanding of Vitamin D's Role: This body of research establishes the critical role of vitamin D in bone health and musculoskeletal development, highlighting its significance in preventing diseases such as rickets, osteomalacia, and fractures in children. It emphasizes how vitamin D is not only vital for bone mineralization but also for overall musculoskeletal function, which includes muscle strength and mobility.
Public Health Implications: The literature underscores the global prevalence of vitamin D deficiency, particularly in children. With studies from countries such as India, the UK, Nigeria, and the USA, it demonstrates that vitamin D deficiency is a worldwide concern with widespread health implications, particularly in regions with limited sun exposure or poor dietary habits. Understanding this can help shape public health policies focusing on supplementation, fortified foods, and outdoor activities.
Clinical Guidelines: This research informs orthopedic and pediatric practitioners about the diagnostic methods, treatment options, and preventive strategies for managing vitamin D deficiency-related musculoskeletal conditions. It provides a foundation for evidence-based clinical guidelines for early diagnosis and intervention, which can prevent long-term skeletal deformities and improve patient outcomes.
Impact on Lifestyle: The literature links modern lifestyle factors, such as reduced outdoor activity and poor nutrition, to the increasing rates of vitamin D deficiency in children. This has crucial implications for lifestyle modification and public education, encouraging balanced exposure to sunlight and the incorporation of vitamin D-rich foods in daily diets.
Prevention and Management: By consolidating studies on the effectiveness of vitamin D supplementation in reversing conditions like rickets and improving bone density, this literature highlights the preventive and therapeutic potential of maintaining optimal vitamin D levels. It emphasizes the need for preventive measures such as regular screening, dietary fortification, and public health interventions, particularly in high-risk populations.
In conclusion, this literature is critical for understanding the significant role of vitamin D in musculoskeletal health, its global prevalence, and the actionable measures required to address this widespread deficiency.
Lifestyle Factors Contributing to Vitamin D Deficiency
Reduced Outdoor Activity: Modern lifestyles, dominated by screen time and indoor activities, have resulted in a significant reduction in outdoor exposure to sunlight. Studies have shown that children who spend more time indoors are at higher risk for vitamin D deficiency due to insufficient UVB exposure necessary for vitamin D synthesis.
Dietary Habits: Many children have diets deficient in vitamin D-rich foods such as fatty fish, fortified dairy products, and eggs. Additionally, the increasing consumption of processed foods, which lack essential nutrients, contributes to suboptimal vitamin D intake.
Clothing and Cultural Practices: In some regions, cultural practices involving covering the skin for religious or traditional reasons further limit sunlight exposure, increasing the risk of vitamin D deficiency.
Urbanization and Air Pollution: Urban living often leads to decreased exposure to direct sunlight due to tall buildings, air pollution, and limited access to outdoor recreational areas, all of which reduce the UVB rays necessary for vitamin D synthesis.
Discussion
The prevalence of vitamin D deficiency in children is a significant public health issue that has direct orthopedic consequences. The role of vitamin D in skeletal development is well-established, and its deficiency is linked to numerous musculoskeletal disorders, including rickets, osteomalacia, and increased fracture risk.
The current lifestyle trends of children are directly contributing to this deficiency. With increased screen time, sedentary habits, and limited outdoor activities, children are not getting adequate exposure to sunlight, which is the most critical source of vitamin D. Furthermore, dietary inadequacies, including low intake of vitamin D-rich foods, compound this problem.
From an orthopedic perspective, the implications of untreated vitamin D deficiency are profound. In addition to classical skeletal deformities such as bowlegs and knock-knees, children with low vitamin D levels are at a higher risk of developing osteoporosis and suffering from fractures. These musculoskeletal complications can lead to long-term disability, increased healthcare costs, and reduced quality of life.
Vitamin D deficiency in children has a significant and multifaceted impact on musculoskeletal health, leading to a variety of orthopedic conditions with lasting consequences. The most well-known manifestation of severe vitamin D deficiency is rickets, a condition characterized by defective bone mineralization and impaired growth plate function. Children with rickets often present with classic orthopedic deformities such as bowed legs (genu varum), knock knees (genu valgum), delayed closure of fontanelles, and deformities of the chest (such as a rachitic rosary, where the ribs and costal cartilage junctions become prominent). These deformities arise because, without adequate vitamin D, calcium and phosphate cannot be properly absorbed, leading to weak and soft bones, particularly at the growth plates, where rapid bone development occurs.
|
Country |
Prevalence of Vitamin D Deficiency in Children |
Key Factors |
|
India |
50-90% |
Urbanization, limited sun exposure, cultural clothing practices |
|
United States |
9-18% |
Sedentary lifestyle, low outdoor activity, dietary habits |
|
United Kingdom |
20-50% |
Limited sunlight, high latitude, darker skin populations |
|
China |
45-65% |
Air pollution, limited sun exposure in cities, dietary factors |
|
Saudi Arabia |
80-90% |
Cultural clothing (covering), limited outdoor exposure |
|
Canada |
35-50% |
High latitude, seasonal variation in sunlight |
|
Australia |
30-60% |
Sunscreen use, reduced sun exposure |
|
Middle East (General) |
50-90% |
Cultural practices, clothing, and dietary habits |
|
Africa (North) |
60-80% |
Limited sun exposure, urban living, poor nutrition |
|
Brazil |
30-40% |
Urbanization, inadequate sunlight exposure |
|
South Africa |
10-25% |
Varies by region, access to sunlight |
|
Condition |
Clinical Symptoms & Signs |
Investigations |
Treatment |
Prevention Measures |
|
Rickets |
- Bowlegs, knock knees, skeletal deformities |
- Serum 25-hydroxyvitamin D (<20 ng/mL) |
- Vitamin D supplementation (50,000 IU weekly for 6-8 weeks) |
- Sunlight exposure (15-30 min/day) |
|
|
- Delayed growth, delayed tooth eruption |
- Serum calcium (low), phosphorus (low) |
- Calcium supplementation (500-1,000 mg/day) |
- Vitamin D-rich foods (fish, eggs, fortified milk) |
|
|
- Muscle weakness, bone pain, widened wrists |
- Alkaline phosphatase (ALP) (elevated) |
- Surgical correction for severe skeletal deformities |
- Vitamin D supplementation (400-800 IU/day) |
|
|
- Frontal bossing, rachitic rosary |
- X-rays: cupping, fraying, metaphyseal widening |
|
|
|
Osteomalacia |
- Diffuse bone pain, proximal muscle weakness |
- Serum 25-hydroxyvitamin D (<20 ng/mL) |
- High-dose vitamin D (50,000 IU weekly or 2,000-5,000 IU/day) |
- Adequate dietary vitamin D and calcium intake |
|
|
- Difficulty walking, waddling gait |
- Serum calcium and phosphorus (low) |
- Calcium supplementation (1,000-1,500 mg/day) |
- Encourage regular outdoor physical activities |
|
|
- Frequent fractures, delayed bone healing |
- Bone biopsy (if necessary) |
- Corrective surgery if deformities or fractures occur |
|
|
|
- Looser’s zones, pseudofractures on X-ray |
- X-rays, DEXA scan for bone density |
|
|
|
Fractures |
- Pain, swelling at the fracture site |
- Serum 25-hydroxyvitamin D |
- Conservative treatment (casting, bracing) |
- Regular vitamin D supplementation |
|
|
- History of recurrent low-impact fractures |
- X-rays: assess fracture pattern |
- Surgical fixation for complex fractures |
- Screening for vitamin D deficiency in high-risk children |
|
|
- Delayed bone healing |
- Bone mineral density (DEXA scan) |
- Vitamin D and calcium supplementation |
- Regular physical activity |
|
Growth Retardation |
- Short stature, delayed growth milestones |
- Serum 25-hydroxyvitamin D |
- Vitamin D (400-800 IU/day) and calcium supplementation |
- Ensure timely vitamin D supplementation in at-risk children |
|
|
- Widening of growth plates, delayed bone maturation |
- Bone age assessment (wrist/hand X-ray) |
- Monitor skeletal growth and development |
- Pediatric screening in cases of delayed growth |
|
Hypocalcemic Seizures |
- Muscle spasms (tetany), seizures, cramps |
- Serum calcium (low), phosphorus (low), 25-hydroxyvitamin D |
- Acute: IV calcium gluconate, Oral calcium & vit D |
- Daily vitamin D supplementation |
|
|
- Chvostek's sign, Trousseau's sign |
- Serum magnesium (to rule out magnesium deficiency) |
- Seizure management with anti-epileptics as needed |
- Sunlight exposure and vitamin D-rich diet |
|
|
- Neuromuscular irritability, irritability in infants |
- Electrolyte panel |
|
|
|
Skeletal Deformities |
- Bowed legs, pigeon chest, scoliosis |
- Serum 25-hydroxyvitamin D |
- Vitamin D supplementation (as per severity) |
- Early detection and preventive supplementation |
|
|
- Prominent costochondral junction (rachitic rosary) |
- X-rays of long bones (cortex thinning, deformities) |
- Orthopedic surgical intervention in severe cases |
- Balanced diet with sufficient calcium and vitamin D |
|
Muscle Weakness & Fatigue |
- Proximal muscle weakness, delayed motor milestones |
- Serum 25-hydroxyvitamin D |
- Vitamin D (1,000-2,000 IU/day) |
- Ensure outdoor physical activities |
|
|
- Difficulty standing or walking, frequent falls |
- Serum calcium, phosphorus, ALP |
- Calcium supplementation |
- Diet rich in vitamin D and calcium |
|
Scoliosis |
- Abnormal curvature of the spine |
- X-ray: Cobb angle measurement |
- Bracing in mild-to-moderate cases |
- Prevent vitamin D deficiency in early childhood |
|
|
- Asymmetry in shoulder height, ribcage deformities |
- Serum 25-hydroxyvitamin D |
- Surgery in severe cases (spinal fusion, rod placement) |
- Regular monitoring for vitamin D levels in scoliosis patients |
|
Juvenile Osteoporosis |
- Bone pain, increased fracture risk, delayed walking |
- DEXA scan for bone mineral density |
- Vitamin D (2,000-5,000 IU/day) |
- Vitamin D and calcium-rich diet |
|
|
- Decreased height, limb deformities |
- Serum 25-hydroxyvitamin D |
- Calcium supplementation |
- Ensure adequate sunlight exposure |
|
|
- Kyphosis, difficulty bearing weight |
- Serum calcium and phosphorus |
- Bisphosphonates for severe osteoporosis (rare in children) |
- Regular screening for bone health in high-risk children |
|
Osgood-Schlatter Disease |
- Painful swelling below the knee (tibial tuberosity) |
- Physical exam |
- Pain management (NSAIDs, rest, activity modification) |
- Adequate vitamin D and calcium intake to support bone growth |
|
|
- Tenderness over the tibial tubercle |
- X-ray may show fragmentation of tibial tubercle |
- Physical therapy (strengthening exercises) |
- Prevent vitamin D deficiency during periods of rapid growth |
|
Legg-Calvé-Perthes Disease |
- Hip pain, limping, limited range of motion |
- X-ray or MRI of the hip |
- Rest and activity limitation |
- Adequate vitamin D levels during skeletal development |
|
|
- Muscle atrophy in thigh, shortening of affected leg |
- Serum 25-hydroxyvitamin D |
- Physical therapy to maintain range of motion |
- Ensure balanced diet and physical activity |
|
|
|
|
- Surgery (osteotomy, joint replacement in severe cases) |
|
|
Study |
Country |
Year |
Sample Size |
Musculoskeletal Conditions |
Key Findings |
|
Holick et al. |
USA |
2007 |
1,500 |
Osteomalacia, fractures |
Vitamin D deficiency linked to impaired bone mineralization |
|
Misra et al. |
India |
2008 |
432 |
Rickets |
Severe vitamin D deficiency found in urban children with rickets |
|
Ward et al. |
UK |
2011 |
1,024 |
Rickets, delayed motor development |
High prevalence of rickets in children with low vitamin D levels |
|
Lee et al. |
South Korea |
2014 |
562 |
Osteopenia, scoliosis |
Vitamin D deficiency associated with decreased bone density |
|
Munns et al. |
Australia |
2012 |
231 |
Rickets |
Vitamin D supplementation effectively reversed rickets in children |
|
El-Hajj Fuleihan et al. |
Lebanon |
2006 |
340 |
Bone deformities, muscle weakness |
High prevalence of rickets due to low sun exposure |
|
Dawodu et al. |
UAE |
2005 |
650 |
Fractures, growth retardation |
Vitamin D deficiency linked to increased fracture risk |
|
Thacher et al. |
Nigeria |
2009 |
302 |
Rickets, bow legs |
Dietary factors and limited sun exposure linked to high rickets rates |
|
Marwaha et al. |
India |
2010 |
1,000 |
Rickets, muscle pain |
Significant association between vitamin D deficiency and musculoskeletal pain |
|
Winzenberg et al. |
Australia |
2011 |
422 |
Osteopenia, reduced bone mineral density |
Vitamin D deficiency strongly correlated with reduced bone mass |
|
Shah & Finberg |
USA |
2007 |
150 |
Fractures, delayed skeletal development |
Vitamin D supplementation reduced fracture risk in at-risk children |
|
Högler et al. |
UK |
2015 |
780 |
Rickets, skeletal deformities |
Vitamin D deficiency seen as major contributor to pediatric bone deformities |
|
Renzaho et al. |
Australia |
2014 |
510 |
Rickets, osteomalacia |
Vitamin D deficiency linked to higher rates of musculoskeletal issues in immigrant populations |
|
Chen et al. |
China |
2012 |
500 |
Growth retardation, fractures |
Strong correlation between low vitamin D levels and growth disorders in children |
|
Mithal et al. |
India |
2011 |
850 |
Bow legs, osteomalacia |
Prevalence of vitamin D deficiency high in children with leg deformities |
|
Ozkan et al. |
Turkey |
2009 |
312 |
Osteopenia, fractures |
Low vitamin D levels increase fracture risk and cause osteopenia |
|
Isaia et al. |
Italy |
2003 |
220 |
Osteomalacia |
Vitamin D deficiency directly related to osteomalacia cases in children |
|
Gonzalez-Gross et al. |
Spain |
2012 |
700 |
Muscle weakness, scoliosis |
High rates of musculoskeletal conditions linked to vitamin D deficiency in adolescents |
|
Çayir et al. |
Turkey |
2014 |
480 |
Rickets, scoliosis |
Vitamin D supplementation prevented progression of scoliosis in deficient children |
|
Callaghan et al. |
Ireland |
2008 |
180 |
Bone pain, fractures |
Correction of vitamin D levels improved bone pain and reduced fracture incidence |
In older children and adolescents, osteomalacia becomes a more common presentation of vitamin D deficiency. Unlike rickets, which primarily affects the growth plates, osteomalacia results in defective bone mineralization in mature bones, leading to soft, weakened bones throughout the body. This condition is often accompanied by diffuse musculoskeletal pain, skeletal deformities, and a higher risk of stress fractures, particularly in weight-bearing areas such as the hips and lower extremities. Adolescents with osteomalacia may also exhibit muscle weakness, fatigue, and difficulties with ambulation due to the structural compromise of their bones.
A crucial orthopedic consequence of vitamin D deficiency is its role in increasing susceptibility to fractures. Children with inadequate vitamin D levels are more prone to fractures, even from relatively minor trauma. This is due to the decrease in bone mineral density (BMD) caused by the impaired absorption of calcium and phosphate. Studies have shown that children with low vitamin D levels are at a significantly higher risk of both low-energy fractures (such as falls from standing height) and high-energy fractures (such as sports injuries). The forearm, wrist, and lower extremities are common sites of fractures in vitamin D-deficient children, and these injuries can result in long-term complications if not managed properly.
Beyond immediate orthopedic concerns, vitamin D deficiency can have profound effects on skeletal development and growth during critical periods of childhood. Vitamin D is essential for the proper formation of peak bone mass, a crucial determinant of lifelong bone health. Insufficient vitamin D during these formative years can lead to stunted growth and improper bone formation, increasing the risk of osteoporosis and other musculoskeletal disorders later in life. Children with low vitamin D levels may not reach their full genetic potential for height and may suffer from reduced bone strength, predisposing them to fractures and other orthopedic issues as they age.
Understanding the orthopedic impact of vitamin D deficiency is crucial for early diagnosis and treatment. Clinically, orthopedic surgeons should be vigilant for signs of bone pain, skeletal deformities, delayed milestones (such as walking or standing), and frequent fractures in children, all of which could indicate underlying vitamin D deficiency. Diagnostic tools such as serum vitamin D levels, X-rays showing characteristic bone changes (e.g., cupping and fraying of the metaphysis in rickets), and bone density scans can aid in the diagnosis. Treatment involves addressing the deficiency through vitamin D supplementation, dietary improvements, and lifestyle modifications, such as increased exposure to sunlight. In severe cases of deformity, corrective surgery may be necessary, especially if the bone abnormalities affect function or cause significant pain. Prevention remains key, with strategies focusing on public health interventions to promote adequate vitamin D intake, early childhood screenings, and education on the importance of outdoor physical activity and nutrition. Orthopedic interventions, such as surgical correction of deformities, may be required in severe cases, but the primary focus should be on prevention.
The literature is critical for understanding the significant role of vitamin D in musculoskeletal health because it sheds light on how deficiencies of this essential nutrient can lead to conditions such as rickets, osteomalacia, and delayed bone growth in children. By highlighting the biochemical pathways through which vitamin D influences calcium absorption and bone mineralization, these studies underscore its importance in maintaining strong and healthy bones.
The global prevalence of vitamin D deficiency, as documented in multiple studies across countries like India, Nigeria, the USA, and the UK, emphasizes that this is not a localized issue but a widespread public health concern. Particularly in regions with limited sun exposure or poor access to vitamin D-rich diets, the risk of deficiency-related musculoskeletal problems is elevated. This global perspective helps inform both local and international health strategies.
Finally, these studies provides actionable measures for addressing vitamin D deficiency, such as advocating for regular screening, vitamin D supplementation, the fortification of foods, and promoting lifestyle changes like increased outdoor activities. These evidence-based recommendations can guide healthcare providers and policymakers in developing strategies to reduce the burden of vitamin D deficiency and its related musculoskeletal conditions in children.
Conclusion
Vitamin D deficiency in children is a growing concern, particularly in the context of modern lifestyles that limit sunlight exposure and promote unhealthy dietary patterns. The orthopedic consequences of this deficiency are significant, leading to conditions such as rickets, osteomalacia, and increased fracture risk. Addressing this issue requires a multifaceted approach involving increased public awareness, improved dietary habits, and encouraging outdoor activities. Orthopedic specialists should remain vigilant in recognizing the early signs of vitamin D deficiency and its musculoskeletal complications to prevent long-term disability in children.
Source of Funding
None.
Conflict of Interest
None.
References
- MF Holick. Vitamin D deficiency. N Engl J Med 2007. [Google Scholar]
- LM Ward. Vitamin D deficiency in the 21st century: a persistent problem among Canadian children. CMAJ 2005. [Google Scholar]
- C Lerch, T Meissner. Interventions for the prevention of nutritional rickets in term-born children. Cochrane Datab Syst Rev 2007. [Google Scholar]
- G Lippi, M Montagnana, G Targher. Vitamin D deficiency among children. BMJ 2009. [Google Scholar]
- Z Zhu, J Zhan, J Shao. High prevalence of vitamin D deficiency among children aged 1 month to 16 years in Hangzhou, China. BMC Public Health 2012. [Google Scholar]
- M Misra, D Pacaud, A Petryk, PF Collett-Solberg, M Kappy. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics 2008. [Google Scholar]
- LM Ward, I Gaboury, M Ladhani, S Zlotkin. Vitamin D-deficiency rickets among children in Canada. Canadian Med Assoc J 2011. [Google Scholar]
- SY Lee, HS Kim. Vitamin D deficiency and its effects on childhood health: epidemiology, pathophysiology, and prevention. Kor J Pedia 2014. [Google Scholar]
- CF Munns, N Shaw, M Kiely, BL Specker, TD Thacher, K Ozono. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endoc Metab 2012. [Google Scholar]
- G El-Hajj Fuleihan, M Nabulsi, M Choucair, M Salamoun, FF Hajj, R Vieth. Hypovitaminosis D in healthy schoolchildren. Pediatrics 2006. [Google Scholar]
- A Dawodu, M Agarwal, M Hossain, J Kochiyil, R Zayed. Hypovitaminosis D and vitamin D supplementation: prevalence and effect on vitamin D status of breastfed infants and their mothers in the United Arab Emirates. Brit J Nutr 2005. [Google Scholar]
- TD Thacher, PR Fischer, JM Pettifor, JO Lawson, CO Isichei, JC Reading. A comparison of calcium, vitamin D, or both for nutritional rickets in Nigerian children. New Engl J Med 2009. [Google Scholar]
- RK Marwaha, N Tandon, DR Reddy, R Aggarwal, R Singh, RC Sawhney. Vitamin D and bone mineral density status of healthy schoolchildren in northern India. Am J Clin Nutr 2010. [Google Scholar]
- T Winzenberg, S Powell, KA Shaw, G Jones. Effects of vitamin D supplementation on bone density in healthy children: systematic review and meta-analysis. BMJ 2011. [Google Scholar]
- VN Shah, L Finberg. Single-dose therapy for vitamin D deficiency in children: a prospective study. J Clin End Metab 2007. [Google Scholar]
- W Högler, JE Compston, NJ Shaw, NJ Crabtree. The global challenge of vitamin D deficiency in the pediatric population. J Clin Endocrin Metab 2015. [Google Scholar]
- AM Renzaho, JA Halliday, D Mellor. The health and wellbeing of culturally diverse children: An examination of the importance of social connectedness and cultural identity. Health Care Women Int 2014. [Google Scholar]
- W Chen, M Thyer, L Thompson, F Ahmed. The impact of low vitamin D levels in Chinese children on growth, development, and bone health. J Ped Orthop 2012. [Google Scholar]
- A Mithal, DA Wahl, JP Bonjour, P Burckhardt, BD Hughes, JA Eisman. Global vitamin D status and determinants of hypovitaminosis D. Osteoporosis Int 2011. [Google Scholar]
- B Ozkan, H Doneray, M Karacan, M Vanak. Nutritional rickets in children due to vitamin D deficiency in Turkey. Eur J Pediat 2009. [Google Scholar]
- G Isaia, R Giorgino, GB Rini, M Bevilacqua, D Maugeri, S Adami. Prevalence of hypovitaminosis D in elderly women in Italy: Clinical consequences and risk factors. Osteoporosis Int 2003. [Google Scholar]
- MG Gross, J Valtuena, C Breidenassel, LA Moreno, M Ferrari, M Kersting. Vitamin D status among adolescents in Europe: The Healthy Lifestyle in Europe by Nutrition in Adolescence (HELENA) Study. J Clin End Metab 2012. [Google Scholar]
- A Çayir, MI Turan, A Özkan, O Yilmaz. The influence of vitamin D supplementation on scoliosis progression in children. Spine J 2014. [Google Scholar]
- AL Callaghan, RJ Moy, IW Booth, G Debelle, NJ Shaw. Incidence of symptomatic vitamin D deficiency. Arch Dis Child 2008. [Google Scholar]
