Introduction
The thyroid gland is a crucial endocrine gland that has a fundamental function in regulating the body's metabolism, growth, and development. It secretes two hormones, namely thyroxine (T4) and triiodothyronine (T3).1
Thyroid hormones (THs) have a crucial function in controlling energy metabolism. Additionally, it has a role in other processes related to the central nervous system (CNS), such as promoting survival, facilitating neuronal development, and regulating energy consumption. A correlation has been shown between thyroid function and symptoms related to the central nervous system, including cognitive decline, depression, and dementia. Literary evidence also demonstrates the impact of thyroid hormones on people with central nervous system disorders, including Alzheimer's disease, epilepsy, depression, and Parkinson's disease.2
The activity of the thyroid gland plays a crucial role in regulating both normal and abnormal biological processes. Research conducted on animal models and humans has shown that thyroid hormones regulate cellular processes associated with aging and the majority of age-related disorders. Multiple studies have shown that even small decreases in thyroid hormone activity are linked to remarkable longevity in both animals and people. However, alterations in thyroid hormones are significant medical disorders that are connected to unhealthy aging and early mortality. Moreover, there is a correlation between hyperthyroidism and hypothyroidism and the occurrence of certain forms of diabetes and malignancies, indicating a substantial intricacy of molecular processes regulated by thyroid hormones.3
Hypothyrodisim
Hypothyroidism is a condition resulting from the thyroid gland's insufficient production of the hormone thyroxine, which is important for regulating biological processes in the body. It is present in around 0.1-2% of individuals and is consequently considered a secondary clinical condition resulting from inadequate thyroid hormone levels, generally caused by hypothyroidism. Hypothyroidism seldom manifests with distinct or severe symptoms. In exceptional instances, hormone synthesis may be adequate, but its effects on the periphery are inadequate. Hypothyroidism may arise either from birth (congenital) or as a result of autoimmune disorders such as Hashimoto's thyroiditis. Hypothyroidism may develop at any age, however it is most prevalent among older individuals. In this scenario, he adopts a nuanced demeanor that might make it difficult to recognize him. Hypothyroidism may be classified into two types: primary, which is caused by an illness affecting the thyroid gland, and secondary, which is caused by a condition affecting the hypothalamus or the pituitary gland. Common clinical manifestations include tiredness, reduced tolerance to cold temperatures, and an increase in body weight. The most serious symptoms are mucous heart disease and myxedema coma, which may be life-threatening if not treated.4
Hypothyroderma, often referred to as severe hypothyroidism, is linked to metabolic abnormalities, such as high levels of cholesterol and elevated levels of low-density lipoprotein (LDL), which raise the risk of developing diabetic mellitus (DM) and issues related to the heart. Partial hypothyroidism is associated with significant complications including neurological and mental health issues, disrupted bone metabolism, an increased risk of developing type 2 diabetes mellitus (T2DM), and various heart-related problems. These heart-related issues include elevated levels of LDL and VLDL, high triglyceride levels, hypertension, atrial heart rhythm disorder, obesity, low levels of HDL, and premature mortality.5
Primary hypothyroidism is characterized by an elevated level of thyroid stimulating hormone (TSH) and a concentration of free thyroxine (fT4) that falls below the normal range. Subclinical hypothyroidism, often indicative of early thyroid dysfunction, is being examined. The most frequent kind of hypothyroidism is acquired primary hypothyroidism, which may be caused by severe iodine shortage, but more usually results in thyroiditis. Levothyroxine (LT4) is the primary therapy and is among the most often given drugs worldwide. Once the TSH and fT4 concentrations have been normalized.6 it is important to note that congenital hypothyroidism is a very avoidable factor that may lead to intellectual impairment. Thyroid hormone is crucial for the normal development of the brain.7
Subclinical hypothyroidism (SCH) is linked to a higher occurrence of atherosclerosis, a condition characterized by the buildup of fat in the arteries. This condition may be triggered or worsened by chronic inflammation, which negatively affects the inner lining of blood vessels. Consequently, it can contribute to endothelial dysfunction and increase the risk of cardiovascular problems.8
Tumor Necrosis Factor Alpha (TNF-ɑ)
TNF-alpha is a cytokine with several immunological and representational functions. Studies have shown that TNF-alpha receptors are present in thyroid follicular cells. TNF-alpha and its receptors have been associated with cytotoxic processes that contribute to the death of the thyroid in autoimmune thyroid disorders. Patients with Graves' illness have revealed increased levels of TNF-alpha in their blood. Research has shown that administering TNF-alpha to people may cause hormonal alterations like those seen in NTDS.9 Multiple studies indicate that TNF-α has a considerable impact on hypothyroidism.10
Recent research has shown that TNF-α is essential for controlling transcription factors in the thyroid gland. TNF-α is a versatile inflammatory cytokine that is primarily generated and released by mononuclear cells, lymphocytes, and several other cell types including thyroid epithelial cells and intrathyroid fibroblasts.11 Several inflammatory markers have been shown to elevate in subclinical hypothyroidism (SCH) and may have a significant impact on the development of insulin resistance condition.12
Oxidative Stress and Hypothyroidism
Thyroid illnesses, including malignancies, autoimmune diseases, and thyroid disorders, have emerged as a significant societal issue due to their increasing prevalence. The latter are becoming more closely linked to oxidative stress. Various methods may be used to detect indicators of oxidative stress, enabling the evaluation of the oxidative profile in individuals with thyroid illness in comparison to those who are healthy. This presents new opportunities for exploring the significance of heightened levels of oxidative stress and damage in individuals with thyroid disorders. The disparity between oxidants and antioxidants is seen throughout many stages and forms of thyroid illness. The gland, a component of the glandular system, utilizes free radicals, namely reactive oxygen species (ROS), for the synthesis of hormones. Thyroid cells secrete enzymes that promote the generation of reactive oxygen species (ROS). Consequently, the body's internal defense system and non-enzymatic antioxidants are crucial in counteracting the surplus ROS that are not utilized in the production of thyroid hormones. They act as a buffer by reducing the concentration of harmful free radicals and maintaining the body's internal equilibrium. Cellular structural damage occurs as a result of an excessive presence of free radicals.13
Thyroid hormones have an impact on the functioning of almost every organ in the body and may cause serious metabolic diseases if there is any malfunction.14 Therefore, the crucial function of thyroid hormones in maintaining metabolic balance is evident. Specifically, these hormones accelerate the breakdown of fats (lipolysis), the breakdown of glucose (glycolysis), and the production of glucose by facilitating the use of carbohydrates by tissues outside of the central nervous system. Furthermore, these hormones enhance the production of calories by boosting the cells' oxygen consumption via their stimulating effects on the growth and development of mitochondria.15 A study conducted by researchers16 shown that even little disruptions in the functioning of the thyroid gland might have significant repercussions on the overall health of the body. Thyroid hormone (T3) has been discovered to have significant impacts on energy metabolism, specifically targeting mitochondria to produce thermogenic effects. Consequently, the disparity in hormone levels seen in thyroid disorders, such as hypothyroidism, disrupts the respiratory chain inside mitochondria. This disruption causes an increased generation of free radicals, ultimately resulting in oxidative stress.
Hypothyroidism and Insulin Resistance
Hypothyroidism is linked to significant peripheral effects on insulin secretion and glucose metabolism. Hypothyroidism, unlike hyperthyroidism, decreases the absorption of glucose from the gastrointestinal tract.17 Furthermore, it is linked to a near-total halt in the generation of glucose by the liver and an elevation in insulin levels.18
Individuals with subclinical hypothyroidism had elevated insulin resistance values for HOMA-IR in comparison to those with hypothyroidism, indicating that reduced levels of thyroid hormones contribute to the development of insulin resistance. Moreover, there was a high correlation between TSH and insulin as well as HOMA-IR readings. Similarly, fT4 and fT3 were strongly connected with insulin and HOMA-IR. Despite the challenge of reconciling the data on the connections between hyperthyroidism and insulin resistance, these relationships indicate that alterations in cellular events related to thyroid hormone (TH) have the ability to contribute to the development of insulin resistance and the removal of glucose, Multiple more investigations have shown a correlation between hypothyroidism and an elevation in insulin resistance.19 Small elevations in TSH levels are linked to subclinical hypothyroidism and are also connected with insulin resistance and hyperlipidemia.20
Materials and Methods
Samples under study
A total of 76 blood samples were obtained from individuals aged (30 – 55) years who have hypothyroidism. Among them, 50 serum samples were taken from individuals with hypothyroidism, while 26 samples were collected from healthy individuals serving as the control group. These samples were collected from outpatient clinics in the city of Samarra between September 2023 and January 2024. The samples were obtained by extracting venous blood, followed by the separation of the blood serum and subsequent performance of the required assays.
The research focused on quantifying the concentration of tumor necrosis factor (TNF-ɑ) using an examination kit developed by the Chinese business Sunlong, which utilizes the enzyme-linked immunosorbent assay (ELISA) technique. The levels of T3, T4, and TSH were determined using an immunosorbent test kit provided by the American business (Monobind), using the enzyme-linked immunosorbent assay (ELISA) method.
Additionally, the levels of superoxide dismutase (SOD), glutathione (GSH), and malondialdehyde (MDA) may be estimated using an enzyme-linked immunosorbent assay (ELISA) test kit provided by the Chinese business BT Lab.
The concentration of insulin in the bloodstream is determined using an ELISA test kit provided by the Chinese business Sunlong.
Statistical analysis
The data from the samples used in the research were gathered and statistically analyzed using the SPSS 27 system, extracting the arithmetic mean and standard deviation. The t-Test was used to examine the disparities between the primary and secondary groups. The groups were chosen based on significant differences, with a probability threshold of (P < 0.05).
Results and Discussion
displays the( mean ± standard deviations) for tumor necrosis factor (TNF-ɑ), T3, T4, TSH, superoxide dismutase (SOD), Glutathione (GSH), and malone dialdehyde (MDA). Additionally, the table includes measurements for insulin levels and P-values for comparing the control group with the patients.
Table 1
Shows the level of (TNF-ɑ), (T3), (T4 ), ( TSH), (SOD), (GSH), (MDA) and insulin for patients with hypothyroidism compared to the control group
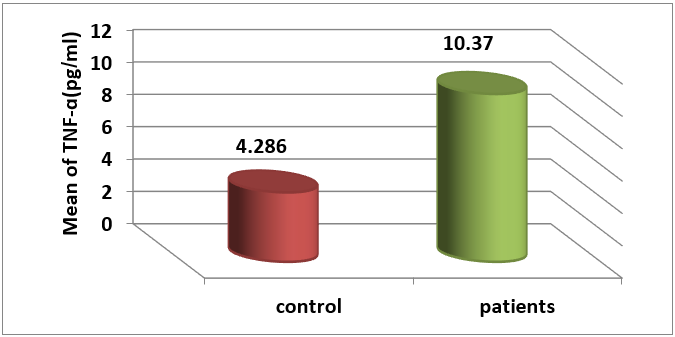
displaysthe( mean ± standard deviation )for the amount of ( TNF-ɑ) in the blood serums of individuals with hypothyroidism, which was measured at (10.37 ± 3.15) pg/ml. In comparison, the level of (TNF-ɑ) in the blood serums of healthy individuals in the control group was found to be( 4.286 ± 1.915)
pg/ml. The findings indicate a significant increase in the level of ( TNF-α) with a probability threshold of( P < 0.05) in infected individuals compared to the control group, as shown in Figure 1,.
The findings of our study align with the research conducted by( Díez) et al. 9 and (Mahaseth) et al,21 which both reported elevated levels of TNF-ɑ in individuals with hypothyroidism.
Tumor necrosis factor (TNF-ɑ), first reported by Carswell et al. in 1975, is a significant cytokine involved in inflammatory and immunological responses.
It is a very potent medium for triggering inflammatory and immunological responses. It has the ability to function autonomously or in conjunction with a diverse range of other cytokines, exerting an influence on the majority of the body's cells. Tumor necrosis factor (TNF) enhances the cytotoxicity and macrophage properties of immune system cells, influences the growth and specialization of B lymphocytes, T lymphocytes, and NK cells, and promotes the production of cytokines. Furthermore, it enhances the production of sticky particles and chemokines that are essential for the gathering of immune cells at the site of inflammation.22
(TNF-ɑ) has a role in the development of thyroid dysfunction, such as autoimmune thyroid disease (AITD). According to many publications, individuals with autoimmune thyroid diseases (AITD) and other thyroid disorders had significantly greater levels of TNF-ɑ concentration and TNF-mRNA in their thyroid gland compared to those without these illnesses. 23 Thyroid cells possess a receptor for TNF on their surface, and it is hypothesized that TNF plays a crucial role in the cytotoxic processes that result in the degradation of thyroid tissue in AITD. 9
Furthermore, TNF suppresses the synthesis of thyroglobulin, 24 diminishes the uptake of iodine by thyroid cells induced by TSH, 25 decreases the function of type 2 deiodinase, leading to a decline in the peripheral production of triiodothyroxine-nine by the thyroid gland, and also decreases the production of TSH-endocrine alone. 26 TNF also impacts the functionality of the hypothalamus-pituitary-thyroid axis. Tumor necrosis factor (TNF) hinders thyrotropin-releasing hormone (TRH), resulting in a decrease in thyroid-stimulating hormone (TSH) release. 27
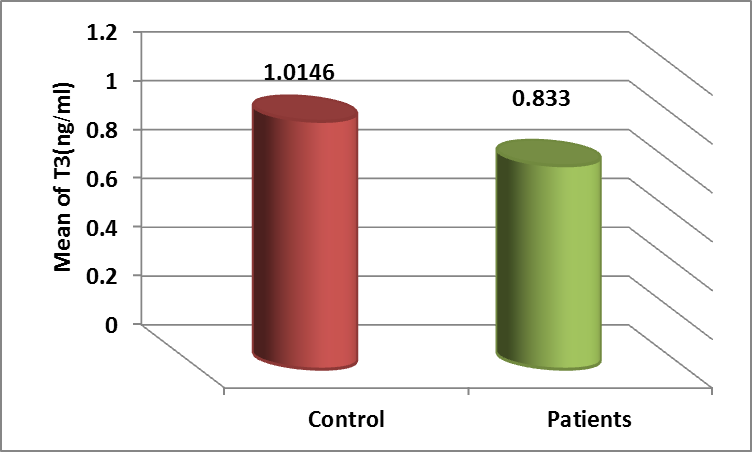
displaysthe( mean ± standard deviation )for the amount of(T3) in the level of (T3) in the blood serums of individuals with hypothyroidism was( 0.833 ± 0.224) ng/ml, while the level in the blood serums of healthy individuals was (1.0146 ± 0.1946 )ng/ml. The foregoing findings indicate a significant drop in the level of (T3) with a probability (P ≤0.05) in infected individuals compared to the control group, as shown in Figure 2,
The results of our investigation align with the discoveries of (Mansoor) et al. 28 and (Khamael) et al. 29 who demonstrated a reduced amount of T3 in individuals suffering from hypothyroidism.
T3 is the primary active form of the thyroid hormone that is responsible for carrying out biological functions. It has a binding affinity to thyroid hormone receptors that is about 10 times greater than that of T4. Approximately 80% of the T3 present in the bloodstream of people originates from T4. T3 has a lower half-life compared to T4. 30
Euthyronine deiodination enzymes are specific proteins called selenoproteins that control the metabolism of thyroid hormones. Type II deiodination enzyme is the primary regulator of the intracellular concentration of triiodothyronine in both the hypothalamus and the pituitary gland. Consequently, it is also the principal regulator of thyroxine production. A deficiency in the enzymatic activity responsible for iodine elimination in euthyroid individuals may lead to decreased sensitivity to the effects of thyroid hormones. Recent scientific literature discusses these deficiencies in conditions known as 'thyroid hormone hypersensitivity syndromes'.31
T3 and T4 have biological effects, however T3 is the active thyroid hormone that attaches to thyroid receptors, whereas T4 is a hormone that has to be transformed to T3 in order to have biological activity.
The thyroid gland synthesizes about 20% of the biologically active hormone T3, with the remaining 80% of circulating T3 levels in healthy individuals being derived from the enzymatic action of iodothyronine diodinase. 32
Type 2 iodothyronine deiodinase (D2) is responsible for the conversion of T4 to intracellular T3 in several human organs, such as the hypothalamus and pituitary gland. The crucial component in regulating TSH release is the intracellular concentration of T3, which is present in both the hypothalamus and pituitary gland. Hence, D2 activity is essential for controlling the hypothalamus-pituitary-thyroid (HPT) axis, both in normal and abnormal circumstances. 33
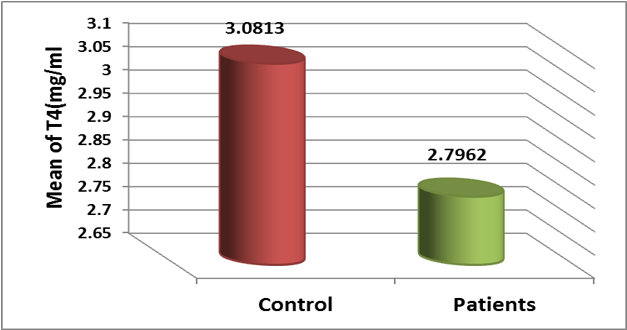
In Table 1, we see that the (mean± standard deviation) for the concentration of( T4) in the blood serums of individuals with hypothyroidism was( 2.7962 ± 0.3653) mg/ml, while in the control group of healthy individuals, it was (3.0813 ± 0.3698) mg/ml. The findings indicate a significant drop in the level of (T4) with a probability (P ≤0.05)in infected individuals compared to the control group, as shown in Figure 3.
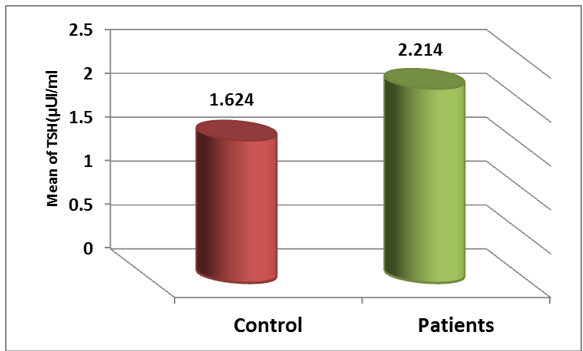
The findings of our study align with those of (Berglund J) et al. 34 and (Muñoz-Ortiz) et al. 35, which demonstrated that hypothyroidism is associated with a reduction in T4 levels. T4, also known as thyroxine, is the primary thyroid hormone synthesized by the thyroid gland. However, its activity is limited, 30 making it a precursor or prohormone. T4 is converted to T3 in peripheral organs, such as the liver, by removing iodine from T4. 36 An elevation in the level of T4 in the bloodstream is anticipated to raise the concentration of T3 and reduce the expression of the TSH gene. Conversely, a decrease in the level of T4 in the blood can have negative consequences, as alterations in T4 concentration specifically impact the Hypothalamus-pituitary-thyroid (HPT) axis solely due to the actions of D2 (iodothyronine deiodinase). 37 The prevailing view suggests that the process of converting T4 to T3 outside of the thyroid gland reduces during periods of severe sickness. This is believed to occur because the activity of the D1 enzyme in the liver and kidneys, as well as the D2 enzyme in skeletal muscle, lowers. 38 In Table 1, the( mean ± standard deviation) of ( TSH) levels in the blood serums of individuals with hypothyroidism was( 2.214 ± 0.3116) μUI/ml, whereas in the blood serums of healthy individuals (control group), it was( 1.624 ± 0.302) μUI/ml. The findings indicate that the level of TSH has significantly increased with a probability level of (P≤0.05) in infected individuals compared to the control group, as shown in Figure 4.
This is supported by( Biondi and Coper), 39 and (Muñoz-Ortiz), 35 who have all highlighted that hypothyroidism is associated with an increase in the concentration of thyroid-stimulating hormone (TSH).
that TSH directly stimulates the synthesis of thyroid hormones. TSH is manufactured and secreted in the anterior pituitary gland, under the influence of thyroxine secretion hormone produced in the brain. The negative feedback regulatory mechanism regulates thyroid metabolism in people with an intact hypothyroid-pituitary-thyroid axis. The pituitary gland functions as a biosensor for thyroid hormone levels and adjusts TSH levels based on input from FT4 and FT3 levels. Inhibiting the synthesis of thyroid hormones results in elevated release of TSH.
The TSH test is primarily used to diagnose thyroid disorders, particularly hypothyroidism, due to various factors. TSH and FT4 concentrations have an inverse association. Furthermore, TSH immunoassays have a sensitivity and specificity above 99%.40
Antioxidants and Their Markers
SOD
displays the(mean ± standard deviation) for the amount of (SOD) in the blood serums of individuals with hypothyroidism was measured to be (76.729 ± 9.534) U/L. In comparison, the SOD level in the blood serums of healthy individuals, serving as the control group, was found to be( 99.896 ± 19.190) U/L. The findings indicate a significant drop in the amount of (SOD) with a probability level (P ≤0.05), in infected individuals compared to the control group, as shown in Figure 5.
GSH
displaysthe( mean ± standard deviation) for the amount of (GSH) in the blood serums of individuals with hypothyroidism, which was (4.472±0.652 )ng/ml. In comparison, the level of GSH in the blood serums of healthy individuals in the control group was( 6.017±0.796) ng/ml. The findings indicate that the amount of GSH has significantly reduced with a probability level (P ≤0.05) in infected individuals compared to the control group, as shown in Figure 6.
MDA
showes (mean ± standard deviation) for the level of (MDA) was( 24.170 ± 3.766 ) nmol /ml in the blood serums of individuals with hypothyroidism, In comparison, the level of (MDA) in the blood serums of healthy individuals in the control group was (12.437 ±3.202) nmol/ml. The findings indicate a significant increase in the level of MDA in infected individuals compared to the control group, as shown in Figure 7. This increase is statistically significant with a probability level of (P≤0.05).
This research showed that hypothyroid individuals had higher levels of MDA and lower levels of GSH and sod compared to the control group, indicating the presence of oxidative stress. Hypothyroidism results in the generation of elevated levels of free radicals via various methods, thereby causing an escalation in oxidative harm and a compromised state of antioxidant defense systems. The results align with the research conducted by( Baskol) et al 41 and (Sankha) et al. 42 which demonstrated that hypothyroidism is associated with elevated levels of malondialdehyde (MDA) and reduced levels of glutathione (GSH) and superoxide dismutase (SOD).
Oxidative stress arises from a compromised antioxidant defense system.43 It has a significant impact on thyroid issues. Hypothyroidism is the most prevalent condition. 44 An insufficiency of thyroid hormones enhances the abundance of free radicals, thus altering their production and leading to oxidative stress.45
Thyroid hormones control the function of antioxidants.46 Glutathione (GSH) has a crucial function in eliminating harmful free radicals and reducing the concentration of lipid peroxide. Glutathione peroxidase (GPx) detoxifies hydrogen peroxide (H2O2). 47 Superoxide radicals undergo decomposition via the action of superoxide dismutase (SOD), resulting in the formation of hydrogen peroxide (H2O2) and oxygen.48
Elevated levels of thyroid-stimulating hormone (TSH) are significant hormonal alterations seen in hypothyroidism, which are linked to heightened production of free radicals. Thyroid hormones have been shown to possess natural antioxidant properties, functioning as antioxidants inside cell membranes.49 In addition, thyroid hormones enhance the rate of mitochondrial biosynthesis, promoting the substitution of older reactive oxygen species (ROS) with freshly produced mitochondria that have a reduced propensity to generate free radicals.50 Furthermore, there is compelling data indicating that thyroid hormones have a significant impact on oxygen consumption inside mitochondria and the metabolism of ATP. Hypothyroidism leads to a decrease in thyroid hormones, which in turn decreases the amount of oxygen consumed.51 produce a substantial amount of reactive oxygen species (ROS), including superoxide and hydrogen peroxide.52
Thyroid-stimulating hormone receptors are present in various cell types, including adipocytes, 53 myocardial cells, 54 lymphocytes, 55 erythrocytes, 56 aortic endothelium, 57 and bone marrow cells. 58 In these cells, thyroid-stimulating hormone can directly cause inflammation, resulting in elevated oxidative stress. TSH directly activates the production of sulfur oxides, which are known to cause inflammation, and also increases the levels of lipid peroxides.59 Thus, in the condition of hypothyroidism, the reduction of thyroid hormone and the surplus of thyroid-stimulating hormone might result in oxidative stress.
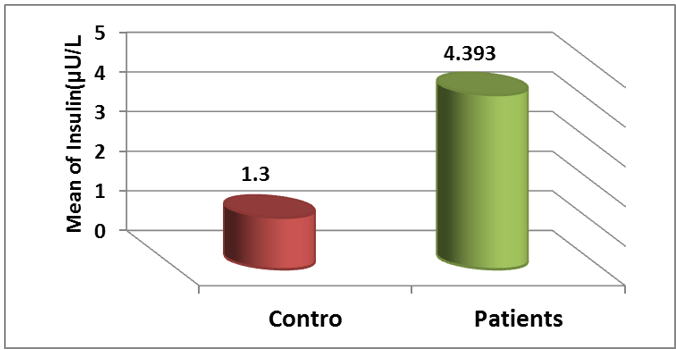
displaysthe( mean ± standard deviation) of the insulin level in the blood serums of individuals with hypothyroidism, which was measured at (4.393 ± 1.921) µ U ⁄L. In comparison, the insulin level in the blood serums of healthy individuals in the control group was measured at( 1.300 ± 0.476) µ U ⁄L. The foregoing findings indicate that the level of insulin has significantly increased in infected individuals compared to the control group, with a probability level of (P≤0.05), as shown in Figure 7.
The results align with the research conducted by (Mahajan) et al.60 and (Yang W )et al.61 since they demonstrated that hypothyroidism leads to an elevation in insulin levels. Hypothyroidism is linked to significant peripheral effects on insulin secretion and glucose metabolism. Hypothyroidism, unlike hyperthyroidism, decreases the absorption of glucose from the gastrointestinal tract.17 Additionally, it is linked to a near-total halt in the synthesis of glucose in the liver and elevated levels of insulin.18
Food restriction triggers an endocrine response that leads to the development of insulin resistance. This insulin resistance allows glucose to be supplied to glucose-dependent tissues, including the central nervous system. 62 Human fasting is linked to reduced levels of plasma glucose. 63 Notably, disruptions in the levels of thyroid hormone in the circulatory system are linked to insulin resistance. Research has shown that thyroid hormone-related diseases play a significant role in the development of insulin resistance. Specifically, studies have shown that undergoing lateral thyroidectomy may lead to improvements in insulin resistance and the restoration of glucose tolerance in diabetic patients with hyperthyroidism. 64 It is not surprising that thyroid disease and diabetes are the two most prevalent endocrine-related disorders treated concurrently in medical practice today. 65 Consequently, it has become evident that there is a connection between TH (thyroid hormone) and insulin signaling, as an imbalance in one can disrupt the regulation of the other. 66 In addition, the role of the thyroid hormone in insulin signaling and glucose metabolism is apparent even in obese individuals. Low levels of T4 within the normal range are linked to a higher incidence of insulin resistance in these individuals.67
There is a strong correlation between the disruption of glucose metabolism and thyroid dysfunctions. research have shown a clear relationship between the severity of the metabolic problem and thyroid dysfunction, with the two being directly proportional. Additionally, other research have indicated that the impact of T3 on glucose metabolism is comparable to that of insulin. 68 Thyroid hormone has the ability to modulate insulin secretion both directly and indirectly. It can do this by decreasing the secretion of insulin that is triggered by glucose, or by diminishing the response of β-cells to increases in cell mass in cases of hypothyroidism and hyperthyroidism, respectively.69
Conclusions
The results of our study show that patients with Hypothyroidism have significantly higher levels of tumor necrosis factor (TNF-ɑ), thyroid-stimulating hormone (TSH), malondialdehyde (MDA), and insulin compared to the control group. On the other hand, there is a noticeable decrease in the levels of triiodothyronine (T٣), thyroxine (T٤), superoxide dismutase (SOD), and glutathione (GSH) in the Hypothyroidism group. These findings indicate a clear state of oxidative stress, as evidenced by the decrease in SOD and GSH levels and the increase in MDA level.