Introduction
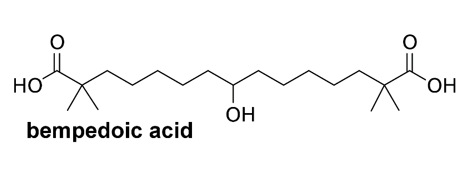
Cholesterol plays several structural and metabolic roles fundamental for human biology, nonetheless too much cholesterol in the blood plasma can lead to pathological consequences. Cholesterol is mainly derived from de novo biosynthesis and the intestinal absorption from the diet. Furthermore, it is known that glucose/insulin promotes cholesterol biosynthesis and its uptake.1 For this reason, blood cholesterol could be monitored already at a relatively young age. Optimal values in human blood plasma are <200 mg/dL for total cholesterol, <100 mg/dL for Low Density Lipoprotein (LDL), and >60 mg/dL for High Density Lipoproteins (HDL). Hypercholesterolemia is a metabolic disorder characterized by the presence of high level of blood LDL. It can be the consequence of an excessive uptake of cholesterol by diet, a genetic syndrome (familial hypercholesterolemia), or other diseases such as type 2 diabetes or hypothyroidism. Heterozygous familial hypercholesterolemia is an autosomal disorder characterized by increased levels of LDL cholesterol. Genetic causes of hypercholesterolemia have been well investigated in recent years. Heritage hypercholesterolemia is characterized by increased serum LDL cholesterol levels, which results in excess deposition of cholesterol in peripheral tissues and in arterial wall, forming plaques. Rather than due to an anomalous enzymatic synthesis or a dietary intake, familial hypercholesterolemia results from defects in the hepatic homeostasis of cholesterol2, 3; it is due to an intricate mechanism of regulation concerning enzymatic biosynthesis, uptake by lipoprotein receptors, storage by esterification, degradation/conversion into bile acids or lipoproteins, and release in the blood. The mainly defects in familiar hypercholesterolemia are mutations/deletions of the liver plasma membrane LDL receptors and over one thousand different mutations in the related genes have been described.4 While a recent review shown in elderly the lack or the inverse association between hypercholesterolemia and mortality,5 according to several studies high LDL cholesterol level is considered among the main risk factor to premature coronary heart disease.2 But not to stroke.6, 7 For this reason, it would be necessary to act promptly with adequate pharmacological therapies to bring very high cholesterol levels to optimal values. In the early 1960s drugs that inhibited cholesterol synthesis became available on the market. Nevertheless, the milestone of hypercholesterolemia therapy is a variety of natural or synthetic drugs developed from 80s called statins (eight introduced to the market, three used in this study, see Figure 1). Several statins are commercialized as a pro-drug (type 1 statins) containing a lactone moiety, which in vivo is enzymatically hydrolyzed to their active hydroxy-acid forms (type 2 statins).8 The inhibitory property is due to the similarity of the open form of statin to mevalonate, the product of the enzyme β-Hydroxy-β-Methyl-Glutaryl-Coenzyme A reductase in the cholesterol biosynthesis (Figure 1). Statins lower total cholesterol/LDL levels from blood and act prevalently in hepatocytes and in the skeletal muscles as competitive and reversible inhibitors of β-Hydroxy-β-Methyl-Glutaryl-Coenzyme A reductase,9 the enzyme key of the mevalonate pathway. Involving in the synthesis of cholesterol and other essential metabolic compounds, including Coenzyme Q10, involved in electron transport-linked phosphorylation.10 Although statins currently constitute the main effective strategy for treating hypercholesterolemia.11 there are two main controversies regarding their use: the resistance and the intolerance to statins that some patients show, and which make this pharmacological intervention futile, if not even harmful. In the intolerance of statins, patients are unable to suffer the therapeutic dose and have adverse effects especially at a muscular level (the most relevant of them is rhabdomyolysis), due to the decreasing in mitochondrial Coenzyme Q10 concentration.12 In the resistance to statins (phenomenon common in about twenty percent of patients), any pharmacological effect is inhibited due to alterations in the absorption, transport, metabolism, or excretion.13 Both phenomena can be associated of polymorphisms in certain genes (has been identified more than 50 candidates) that affect statin pharmacodynamics and pharmacokinetics.
Figure 1
Chemical structures of the statins used in this study. Monacolin K (natural compound obtained by fermentation of white rice by Monascus purpureus or other species of mold) and lovastatin (obtained synthetically) present the same structure.14
Case Presentation
Patient 1. S.T. is a woman born in 1958 and always lived in the countryside; she is a housewife with normal level of physical activity that her employment requires. Her parents both died of acute myocardial infarction, the mother at 45-years-old and the father at 52-years-old, nothing is known about their anamnesis. She follows a normocaloric balanced diet and was a heavy smoker until 60-years-old. The patient 1 uses limited alcohol and coffee, has normal glycemia (February 2024: 106 mg/dL) and blood pressure (January 2024, sitting, left arm: 117/71mmHg). The weight is 42 kg and menopause occurred at 50-years-old. Between 2021 and 2022, she underwent four inoculations by SARS-CoV-2 mRNA vaccine (Biontech). During the present investigation, she was also diagnosed with hyperthyroidism, scleroderma, and cholelithiasis, treated in resolutive manner, respectively, by methimazole, pentoxifylline, and ursodeoxycholic acid.
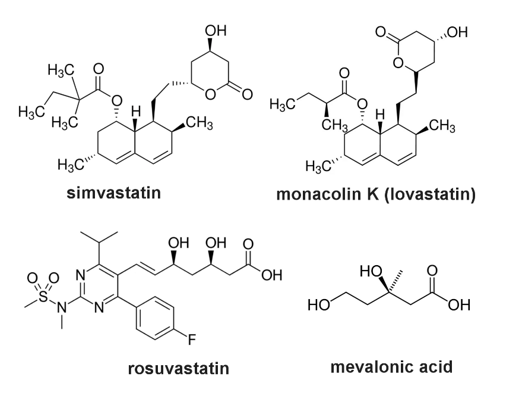
At 50-years-old (2008), during a routine checkup the patient recorded total cholesterol/LDL values higher than normality (Figure 2), while HDL and triglycerides were normal. After one month of ineffective intake of yogurt enriched with plant sterols, the family doctor, considering an action to correct this disorder, decided to start a pharmacological treatment with 20 mg daily of simvastatin, monitoring periodically the outcome of the therapy. Despite the absolute adherence to therapy, the treatment shown quite fluctuant and not satisfactory effects on the levels of total cholesterol/LDL (Figure 2) and the same physician decided to correct the therapy by prescribing fermented red rice nutraceutical (formulation 1, see Table 1) equivalent to 10 mg daily of monacolin K (chemically equivalent to lovastatin). At the same dosage, in previous studies the reduction of total cholesterol/LDL was approximately by 20 %.15
In 2022, as she didn’t achieve an acceptable and stable improvement, the new family doctor decided for a novel therapy with 5 mg daily rosuvastatin. After having verified for several months its ineffectiveness, the dosage was increased to 10 mg and then 15 mg, but the dysfunction remained with a fluctuation independent to dosage (Figure 2).
Figure 2
Diagram reassuming the case of patient 1. Total cholesterol analyses from serum were performed by the Roche enzymatic-colorimetric method. The results (expressed as mg/dL of total cholesterol) were reported in the histogram year by year. The composition of nutraceutical preparation containing monacolin K (formulation 1) is described in Table 1. No side effects were found with any drugs at any dosage.

Given this standoff phase, not immediately serious but which represents a sword of Damocles due to the consequences that may arise in the long term, the family doctor changed the therapy and prescribed ezetimibe in combination with rosuvastatin (both 10 mg/day) by virtue of their concerted action as cholesterol lowering. Ezetimibe (Figure 3) is a potent inhibitor of Niemann-Pick C1-like 1, a cholesterol receptor highly expressed on the surface of enterocytes and involved in LDL intestinal absorption and transport to the liver.16 Ezetimibe allows the patient refractory to statins to achieve their recommended LDL goal. The action of ezetimibe results in a reduction of LDL content packaged into chylomicrons, which subsequently decreases the amount of cholesterol delivered by themselves chylomicrons to the liver. The decreased source of cholesterol from intestine to liver causes upregulation of LDL receptors on hepatocytes, which promotes the cholesterol uptake from blood plasma, bringing it to normal values.17 The exact mechanism by which ezetimibe reduces the intestinal adsorption of cholesterol is not completely established, but more hypotheses are proposed, included its capacity of changing the shape of Niemann-Pick C1-like 1 receptors interfering with the binding to cholesterol. Co-administration of ezetimibe and rosuvastatin (both 10 mg/day) induces a significant reduction of LDL than an equal dosage of rosuvastatin alone (-60% and -45% respectively), while ezetimibe alone, at the same concentration, induces a decrease of 15%.18 Ezetimibe is, de facto, an adjuvant for the statin therapy and, despite the apparent synergistic action of the two class of drugs, no pharmacokinetic interaction between both is established. After two months of the above-mentioned therapy, the analysis of total cholesterol/LDL indicates the restoration to the commonly acceptable level (total cholesterol: 195 mg/dL), never shown in the last 15 years during this set of analysis (Figure 2). The lowering of total cholesterol stands at 28% than to that found without any therapy; therefore, the decrease is approximately half than to that reported in the literature.18 This phenomenon is understandable since the patient shows total resistance to statin therapy, including rosuvastatin. This feature, despite being notoriously widespread, was not included in the published study.
The good conclusion of the therapy excludes the ultimate use of bempedoic acid (Figure 4), a new lowering cholesterol pro-drug, used in combination with a statin, approved in 2020 for marketing in European Union, which represents the last therapeutic option alternative to statins but without (or with less of) their common adverse effects and pharmacological ineffectiveness. This molecule, after activation in the liver by Coenzyme A of one of their two equivalent carboxylic moieties, blocks the cascade devoted to cholesterol biosynthesis, as inhibitor of citrate lyase, the enzyme involved in the synthesis of acetyl coenzyme A, the first reaction of this metabolic way.19
Patient 2. C. A. is a male born in 1980 and is the only descendant of patient 1. He carries out considerable physical activity consisting of one hour of cycling in the street per day, at least six days a week, limited alcohol and coffee. He has a very healthy diet, predominantly vegetarian. The body mass is 50 kg, he doesn’t smoke and has a normal glycemia (November 2023: 82 mg/dL) as well as blood pressure (November 2023, sitting, right arm: 110/70 mmHg). In the paternal side of the family there is no recurrent hypercholesterolemia requiring pharmacological treatment; the paternal grandfather had a myocardial infarction at 60-years-old with a positive prognosis. Patient 2 has been in good health, except for several episodes of renal colic in 2008, with final expulsion of some calcium oxalate stones. The problem never recurred. Between 2021 and 2022 he underwent to three inoculations by SARS-CoV-2 mRNA vaccine (Biontech), despite, in November 2022, he contracted Covid-19 with rather mild symptoms resolved within ten days, followed by long-Covid, which lasted for at least six months.
In 2018, a routine hematological analysis revealed quite high values of total cholesterol/LDL than normality (Figure 5), while HDL was normal. The same things recurred in the following years, but the practitioner did not consider an action because the values were acceptable. In 2023 the new family doctor prescribed a therapy based on fermented red rice (formulation 1, see Table 1) equivalent to 5 mg daily of monacolin K. Two months after starting the therapy, total cholesterol/LDL values lowered of 26%, reaching normal levels (Figure 5). Previous study with monacolin K administrated at similar concentration proved a total cholesterol/LDL lowering effect approximately of 15%.20 Given the notable response to the drug, the doctor decided to reduce the daily dosage of monacolin to 2,9 mg, always in the form of fermented red rice (formulation 2, see Table 1). After one month of therapy, the hematic concentrations of total cholesterol/LDL were still at the levels already described (Figure 5 ).
Figure 5
Diagram reassuming the case of patient 2. Total cholesterol analyses from serum were performed by the Roche enzymatic-colorimetric method. The results (expressed as mg/dL of total cholesterol) were reported in the histogram year by year. The compositions of different formulations are described in Table 1.
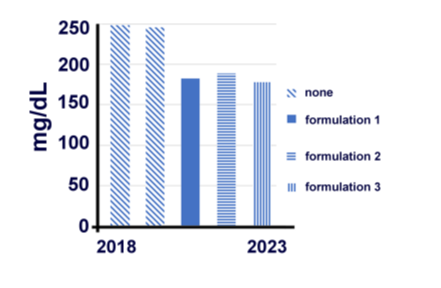
The above-mentioned results obtained after therapies by commercial supplement could not be rigorously useful to establish if the fermented red rice (monacolin K and other monacolins) has an effective part in the lowering of total cholesterol/LDL. In fact, the composition of these commercial formulations contains, also a fermented red rice, other botanical preparations and active ingredients known to have some adjuvant action in the regulation of blood cholesterol, but which often have not been fully evaluated individually or in combination. For this reason, the physician prescribed a bicomponent supplement containing fermented red rice, corresponding to 2,9 mg/day of total monacolins plus 20 mg/day of Coenzyme Q10, to remedy the typically deficit of this metabolite during statin 21 (formulation 3, see Table 1 ). The results obtained taking formulation 3 are like those previously described, showing non-statistically differences.
Table 1
Formulation of the three commercial fermented red rice preparations used in this report and its daily dosage. Formulation 1 is referred to patient 1 (10 mg) and patient 2 (5 mg), formulation 2 and formulation 3 is referred to patient 2. No side effects were recorded with any preparation at any dose.
Formulation of the three commercial fermented red rice preparations used in this report and its daily dosage. Formulation 1 is referred to patient 1 (10 mg) and patient 2 (5 mg), formulation 2 and formulation 3 is referred to patient 2. No side effects were recorded with any preparation at any dose.
Discussion
In the collective imagination, myocardial infarction has always been considered the most shocking form of death, because it strikes suddenly, often without leaving any escape. It is only in recent decades, with scientific advancement in the medical field, that its causes have been investigated and identified. Hypercholesterolemia seems to be one of the main modifiable risk factors for the onset of myocardial infarction. Heritable hypercholesterolemia is not due to the incorrect intake of total cholesterol/LDL from the diet; it comes instead naturally synthesized by enzymatic way, but the liver is unable to recycle from plasma the natural supply that is constantly produced by cells. This route is subject to genetic predisposition, there is therefore a strictly familiarity with this event.22
We considered two clinical cases: patient 1 (mother) presented with a complex set of comorbidities resolved by specific pharmacological treatments, and patient 2 (son) essentially healthy. In both cases, total cholesterol/LDL levels are significantly higher than normal, but not so elevated as to represent an immediate health risk. Statins are considered the “gold standard” in lowering total cholesterol/LDL from blood. There are eight different commercial formulations of statins, so medical prescriptions can depend on the tolerance and effectiveness of the single patient treated. Resistance to statins is well known and genetic predisposition plays a fundamental role. In this study the patients show a significant level of total cholesterol/LDL but only patient 1 (mother) presents resistance to all the statins that have been prescribed, both type 1 and 2 (simvastatin, monacolin K, and rosuvastatin), which makes the disorder essentially intractable using this therapeutic strategy; while patient 2 (son) responds very well even to relatively low dosage of monacolin K, no showing resistance to the drug, unlike the mother.
Monacolin K and lovastatin have the equivalent chemical structure, but the first is obtained by fungal fermentation of the white rice and the second synthetically. In addition to monacolin K (content of 0,3 % w/w in fermented red rice, reported by,20 this dietary supplement contains eight smaller quantities of monacolin-related substances (for each, content of 0,01-0,1 % w/w in fermented red rice, reported by20 with the ability to inhibit β-Hydroxy-β-Methyl-Glutaryl-Coenzyme A reductase, the enzyme implicated in the rate-determining step of cholesterol biosynthesis. Fermented red rice have paradoxically a major pharmacological effect if compared to the one of its contents of monacolin K alone or the equivalent lovastatin. This phenomenon is unlikely to be solely to monacolin K, but rather to result from a combination of action of the different monacolins in the formulation, which, de facto, have a pharmacological power equal or superior to monacolin K (lovastatin) itself.
The use of fermented red rice as dietary supplement has become very popular in recent years for the false concept that it is essentially harmless and with no health risks. It is also bizarre that it can be bought without any medical prescription (it can be easily purchased at supermarkets) which is instead strictly necessary to buy lovastatin and the other statins, since they are chemically equivalent or similar.
In 2018, following a request from European Commission, the European Food Safety Authority (EFSA) published a report about the safety of fermented red rice as dietary supplement. The paper concluded that: “The panel considered that available information on the adverse effects reported in human were judged to be sufficient to conclude that monacolins from fermented red rice when used as food supplements were of significant safety concern at the use level of 10 mg/day”. However, in same report continues: “The panel further considered that individual cases of severe adverse reactions have been reported for monacolins from fermented red rice at intake levels of as low as 3 mg/day”. The Panel concluded that exposure to monacolin K from fermented red rice could lead to severe adverse effects on musculoskeletal system, and on the liver, exactly as for lovastatin. Based on the information available, “The Panel was unable to identify a dietary intake of monacolins from fermented red rice that does not give rise to concerns about harmful effects to health, for the general population, and as appropriate, for vulnerable subgroups of the population”.23 For these reasons, from June 2022, the European Commission allows on the territory of the European Union the sale of products based on fermented red rice containing monacolin K less than 3 mg per dose. However, it is not clear the scientific basis from which this decision draws inspiration, because on the one hand 3 mg daily dosing of monacolin K generally does not a satisfactory lowering of total cholesterol/LDL in people with severe hypercholesterolemia, on the other this quantity is not totally free of side effects, especially for vulnerable people. This approach, at least, focuses a certain attention on the use and, sometimes, abuse of this nutraceutical at the top for managing mild to moderate hypercholesterolemia.
The controversial link between hypercholesterolemia and infarction (as well as debated statin therapy to lower cholesterol plasma levels) is largely disclosed by the scientific literature and could find a touchstone in an ancient Hindu fable, which sees as protagonists several blind men struggling with an elephant. Because this people have never met an elephant before, they learn to conceptualize it simply by touching it, comparing the various experiences they have with the same animal. Each blind man feels a different part of the elephant's body, but only one part, such as side, trunk, tusk or ear. Therefore, they describe the elephant based on their limited experiences and pictures differ from each other. The moral of the fable is that humans tend to claim absolute truth based on their limited and subjective experiences, which could be very seductive but potentially mislead, often ignoring other people's views that may really be the right one.
Ethics Declarations
The authors currently have no conflict of interest in this matter. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This report is not now being considered for publication by another journal. All authors contributed to the study conception and design.