Introduction
Mood is a sustained pervasive emotional response which has been known to man since antiquity. It magnifies human experiences to larger than life proportions. Normal or an average mood is the state of not feeling particularly euphoric or sad except under right circumstances. Superficially, depression is viewed as extremes of the normal fluctuation in mood. But, clinical depression is mo re than extremes of normal mood, it represents syndromes in which in addition to mood, there are disturbances in thought, psychomotor state, behavior, motivation, physiology and psychosocial function.1
The term “depression”, variably defines an affected mood state, a disorder or a specific entity which is defined as depressed mood characterized by sadness, indifference, apathy or irritability and is usually associated with changes in sleep pattern, appetite, motor agitation, fatigue, impaired concentration and decision making.1
Depression is considered as one among the major health problems world wide as it is highly prevalent in general population and leads to significant loss of quality of life and social functioning in the affected individual.
According to WHO, depressive disorders currently rank fourth among the leading causes of disease burden, and they are even estimated to rank second in the world and first in high income countries by the year 2030.2 The estimated risk of depression is 8-12% in males and is 20-26% in females. It is twice more common in women than in men and increases with age in both sexes. However, the overall life-time risk of major depression or depressive episode is about 8%. The impact of depressive disorders on public health is substantial and increasing. World health report 2001 estimated that there are 121 million people worldwide suffering from depression.3 As a consequence of their negative effects on individual and public health, depressive disorders have a significant impact on the economy.4
The health hazards of high serum lipid levels have been well established. Recent research have shown that very low cholesterol levels may be just as unhealthy as very high total cholesterol levels. Adequate cholesterol is so essential that our body warns with depression if serum cholesterol level is too low. The lower the cholesterol level, the deeper is the depression. Cholesterol is especially abundant in the nervous system and is important in many aspects of cellular structure and function. It affects the fluidity of cell membranes, membrane permeability and exchange processes. It has been postulated that changes in the cholesterol content of the synaptosomal membrane leads to decrease in the number of serotonin receptors due to decrease in cholesterol concentration leading to depression.5
Number of researchers recorded relation between acute depression and reduced levels of cholesterol in blood.6,7,8,9 In contrast to other studies, a study by Ledochowski M, et al. showed an association between increased serum cholesterol and signs of depressive mood.10 Several reasons might be contributory for these varied results such as study designs differed widely, studies included different set of age groups, sample size differed widely. In view of the contradictory findings in relating depression with serum lipid levels; we intended to study the association between serum lipid profile and depression.
Materials and Methods
A case control study was carried out over a period of one year. The patients were selected from the department of Psychiatry attending outpatient and inpatient department of KIMS, Hubballi with a study group consisting of 100 cases of depression and 100 healthy individuals as controls. The cases and controls belong to the age group of 20-60 years. After taking informed consent, both cases and controls were interviewed to obtain relevant data. Based on inclusion and exclusion criteria, minimum of 100 cases were selected and 100 age and sex matched healthy individuals were taken as controls.
Inclusion criteria
100 diagnosed cases of depression with symptoms present more than 2 weeks based on International classification of diseases, tenth revision, diagnostic criteria for research (ICD-10-DCR) criteria for diagnosis of depression.
Cases belong to the age group of 20-60 years.
Healthy age and sex matched normal individuals without depressive symptoms and any other psychiatric illnesses, screened by Mini International Neuropsychiatric Interview (M.I.N.I) were selected as controls.
Exclusion criteria
Subjects with any organic brain lesions.
Subjects with other major illnesses like cardiovascular diseases, hypothyroidism, liver disorder, diabetes mellitus and malignancy.
Subjects on cholesterol lowering drugs.
Pregnancy, lactation, use of OCPs.
Smoking, alcohol abuse or dependence.
History of recent significant weight loss.
Method of collection of data
Cases were selected based on ICD-10 criteria for depression and controls were screened by using Mini International Neuropsychiatric Interview (M.I.N.I).11 Severity of depression was rated on 21 item Hamilton Rating Scale for depression (HRSD) questionnaire rated on 0-4 likert scale, according to which, depressives were graded as no depression (0-6), mild (7-17), moderate (18-24) and severe (>24) depression.12
Methodology
After informed consent, about 5 ml of venous blood was drawn from the subjects after 8hrs of fasting from ante cubital vein under aseptic precautions in vacutainer with clot activator for both cases and controls. The serum was separated by centrifugation and used for analysis of total cholesterol (TC) by cholesterol oxidase phenol 4-aminoantipyrine peroxidase (CHOD-PAP) method, triglyceride (TG) by glycerol phosphate oxidase peroxidise (GPO-POD) method, LDL cholesterol (LDL-C) by direct assay method and HDL cholesterol (HDL-C) by phosphotungstic acid method.13
Table 1
Descriptive statistics of cases
Statistical analysis
Results were expressed as mean ± SD. Student’s independent t-test was used for comparing the means of two groups. Relationship between parameters was assessed by Pearson’s correlation coefficient using SPSS (Statistical package for social sciences) software version 19.0. For all the tests, the probability value (p-value) of less than 0.05 is considered statistically significant.
Results
Results we re expressed as mean ± SD. Table 3 depicts the descriptive statistics of cases and controls. The comparison statistics of serum total cholesterol, TG, LDL-C and HDL-C are depicted in their levels in Table 4. The correlation statistics between TG, TC, LDL-C, HDL-C and HRSD scores is shown in Table 5.
Discussion
In the present study, serum TC levels was significantly decreased in cases as compared to controls (p<0.001) where as there was no significant difference found in serum TAG, LDL-C and HDL-C levels in cases as compared to controls On correlation analysis, we observed that there was negative correlation between TG, TC, LDL-C and HRSD scores which was statistically significant (<0.05). Further we observed that this significance of correlation with TC was highly significant (p <0.001) which indicates that the serum TC level is negatively proportional to the severity of depression. That is, the patients with severe depression have reduced level of total cholesterol. This is due to changes in the cholesterol content of the synaptosomal membrane and a decrease in the number of serotonin receptors due to a decrease in cholesterol concentration. Studies have provided explanation for a relationship between low cholesterol and mood. It has been assumed that changes in cholesterol level influence the stability and permeability of cell membranes. Marenah et al. tested this hypothesis by studying the lipid content and fluidity of blood mononuclear cells in healthy male volunteers with a wide range of cholesterol levels (3.2-10.0 mmol/l) in their study.14 Changes in cholesterol level in these studies lead to a wide range of effects, mainly on membrane protein function and thus, in general, on membrane permeability. Although one could speculate that changes in membrane permeability could induce changes in tryptophan transport over the blood-brain barrier, it is not obvious that membrane permeability is strongly influenced by low serum cholesterol levels. On the basis of the meta-analysis, Engelberg proposed the theory which states that cholesterol in biological membrane (phospholipid layer) is in free exchange with serum cholesterol and reduction in serum cholesterol levels results in decrease in cell membrane cholesterol and lowers the lipid microviscosity, which leads to decreased exposure of protein serotonin receptors on membrane surface in turn leading to decreased uptake of serotonin from blood and entry into brain cells leading to depression.5
Table 4
Comparison betwee n serum levels (mean ± SD) of T G, TC, LDL-C, HDL-C in cases and controls
Table 5
| Parameters | HRSD scores | |
| r value | p value | |
| TG | -0.28 | 0.005 * |
| TC | -0.87 | 0.000 ** |
| LDL-C | -0.33 | 0.001 * |
| HDL-C | -0.09 | 0.360 |
Pearson’s correlation co-efficient between serum TG, TC, LDL-C and HDL-C levels with HRSD scores of depression
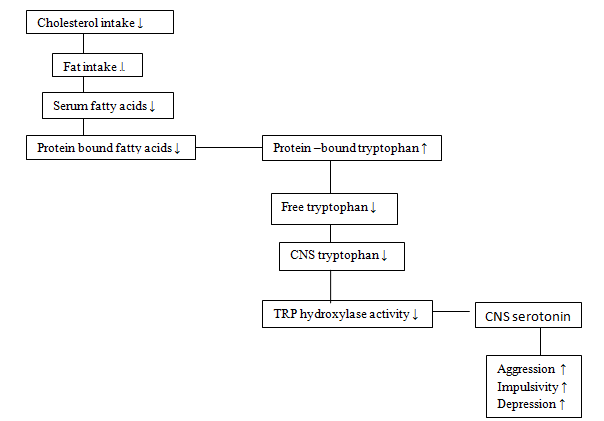
Another possible mechanism related with low dietary intake of cholesterol is that the reduction in dietary cholesterol intake may reflect a reduction in overall fat intake. This results in a decrease in serum fatty acids. Since fatty acids and tryptophan (the serotonin precursor) compete for a binding site on serum albumin, more tryptophan will be bound. As the enzyme catalyzing the synthesis of serotonin (tryptophan hydroxylase) is unsaturated with tryptophan, a decrease in free serum tryptophan will lead to a corresponding decrease in brain serotonin synthesis which leads to depression and vital exhaustion15 (Figure 1). This mechanism was proved in the study by Steegmans.16 It should be noted that this hypothesis is mainly applicable to cholesterol that is lowered through diet. This could also provide an explanation for the possible association between a naturally occurring low cholesterol levels and depression, when supposing that the low cholesterol concentration is attained by long-term low fat diet.
Our study is supported by the similar study by Lori Brown, et al reported an association between low serum cholesterol concentration and severe depressive symptom in an elderly population.17 Besides, some trials showed that clinical recovery may be associated with a significant increase of total cholesterol.8
Another study conducted by N. Sheikh, A. Farhadi Nasab, M. Araghchian and Kh. Mani Kashani concluded that there was no significant relationship between age, sex and triglyceride levels with depression (P >0.05), but there was a significant relationship between low cholesterol and depression (P <0.05).18 Study by Maimanee TA, Al- Hazmi on relationship between blood cholesterol and depression showed a close relationship between acute depression and reduction in blood cholesterol (less than 160 mg/dl). This study was compatible with others that confirm the hypothesis declaring the close relationship between acute depression and low blood cholesterol.7
Even though from our study we show that serum total cholesterol can be studied further as an early biomarker in the screening of depression patients, there are few limitations of the current study such as the association of levels of cholesterol with the progression of disease was not studied. Hence, it is difficult to establish a causal relationship between total cholesterol level and depression. Also, the study did not include a long-term follow-up to know the changes in TC levels following treatment.
Conclusion
We conclude from our study that there is significant association between serum total cholesterol levels and depression. Thus, the patients with low serum cholesterol levels should be screened for depression and further studies may establish serum cholesterol as a new biological marker for depression. Also, there is a need in monitoring of cholesterol levels in patients on long term use of cholesterol lowering drugs. The physician should be aware of potential depressive symptoms in patients with known chronic low cholesterol levels.
Future scope: Further studies are required for definitive establishment of causal relation. There is a need to study the total cholesterol level in association with CNS serotonin activity in spinal fluid through lumbar puncture. It is necessary to obtain CSF samples for assessment of various parameters such as CNS Tryptophan, Tryptophan Hydroxylase and Serotonin levels. Detection of changes in brain by this methodology on the basis of their cholesterol levels could provide important causal information.