- Visibility 67 Views
- Downloads 9 Downloads
- DOI 10.18231/j.ijcbr.2019.064
-
CrossMark
- Citation
A study of thyroid profile in depression
- Author Details:
-
Latha P
-
Ravi B V *
-
Lakshmi Pandith
Introduction
Depression is a common serious mental illness with major health, economic, and social consequences. The World Health Organization (WHO) defines depression as a disorder characterized by sadness, loss of interest or pleasure, feelings of guilt or low self-worth, disordered sleep or appetite, decreased energy and poor concentration. Depressive feelings and symptoms can be acute or chronic, often recurrent and can considerably impair an individual's ability to carry out activities of daily living. In its most extreme cases, depression can lead to suicide.
Major Depressive Disorder (MDD), is diagnosed when an individual experiences a severely depressed mood and activity level that persists for two weeks or more.[1],[2] The worldwide prevalence of clinical depression in the general population is estimated between 3 and 10%, and is increased among individuals with chronic disorders, ranging from 22 to 46%.[3]
The diagnosis of depression and its grading as mild, moderate and severe was done on the basis of ICD-10, DCR as developed by the division of Mental Health of the World Health Organization (WHO, 1992). As a rating scale, Hamilton Rating Scale for Depression (HAM-D) was used for comparison with the clinical diagnosis of depression.
Prevalence of depressive symptoms is close to 50% in people with hypothyroidism and 28% with hyperthyroidism.[4]
Both excess and insufficient thyroid hormones can cause mood abnormalities including depression that is generally reversible with adequate thyroid treatment.[5]
Clinical hypothyroidism is a condition which is characterized by elevated levels of the thyroid stimulating hormone (TSH), additional low levels of triiodothyronine (T3) and thyroxin (T4). Subclinical hypothyroidism is defined as a state of increased serum TSH levels with circulating T4 and T3 concentrations within the population reference.[6] Depressive symptoms are frequently an early or first manifestation of thyroid disease. Hypothyroidism can produce signs and symptoms of depression and can co-exist as a secondary illness in depressed patients.[6] Subclinical hypothyroidism may lower the threshold for occurrence of depression.[7]
The thyroid hormone has complex interactions with the catecholamines, whereas its effects on serotonin systems are more reproducible and suggest that thyroid hormone levels may have an inverse relation to brain serotonin function, mediated by changes in serotonin receptor sensitivity.[8]
Materials and Methods
The study was carried out in 30 newly diagnosed depressed subjects and 30 non-depressed healthy controls who attended the outpatient department of Psychiatry of Kempegowda Institute of Medical Sciences, Bangalore during the year 2014-15. The institutional ethical committee approved the study protocol. Informed consent was obtained from all the participants. The diagnosis of Depression as per on basis of International Classification of Diseases(ICD-10), Diagnostic Criteria for Research(DCR) as developed by the division of mental health of the WHO (1992). As a rating scale, Hamilton Rating Scale for Depression is used for comparison with the clinical diagnosis of depression and to grade the severity.
Age and Gender matched healthy subjects in age group of 18 to 60 years were considered as controls.
Patients with diabetes, hypertension, renal, liver disorders, infection, autoimmune disorder, other psychiatric disorders, drugs such as antipsychotics, OCP, substance use, anti thyroid drugs and those who are on hormone replacement, pregnant and lactating subjects were excluded.
A pre-structured and pre-tested proforma was used to collect the data. Baseline data including age, BMI, detailed medical history, clinical examinations and relevant investigations were included as part of the methodology.
Fasting blood samples were drawn to measure serum thyroid stimulating hormone(TSH), Triiodo thyronine(T 3), Thyroxine(T 4), glucose, urine sugar & albumin.
Serum T3,T4,TSH was measured by Enhanced Chemiluminescence Immunoassay (ECLIA) on Cobas e601 analyzer, Roche diagnostics. FBS by GOD/POD method, Urine glucose & albumin by dipstick method. Body Mass Index was calculated using Weight in Kg / (Height in meter).[2]
Statistical analysis
SPSS software version 22 was used for statistical analysis. Comparison between both groups was performed using Fisher's Exact test, Mann Whitney test, Kruskal Wallis test, Chi square test. Correlation analysis were done using spearman's rank order correlation coefficient. A p value of ˂ 0.05 was considered statistically significant.
Results
Results on continuous measurements are presented as Mean± SD. The basic characteristics and normal distribution of biochemical parameters in cases & controls are depicted in [Table 1].
The cases and controls are divided into 4 groups (18-30years, 31-45yrs, 46-60yrs) Maximum numbers of cases belonged to the age group of 18-30yrs (53.3%). The mean age between the cases and controls was not statistically significant (P>0.05) with higher percentage of females. BMI recorded in cases than in controls and in severe depression compared to other degree of depression showed slightly higher mean and was statistically insignificant.
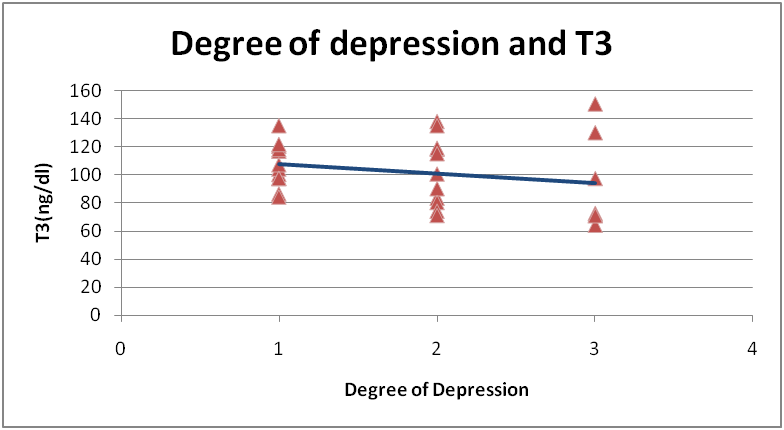
Higher mean T3 was recorded in controls compared to cases and in mild depression compared to other degree of depression but the difference between the two groups and degree of depression was not statistically significant (P˃0.05).
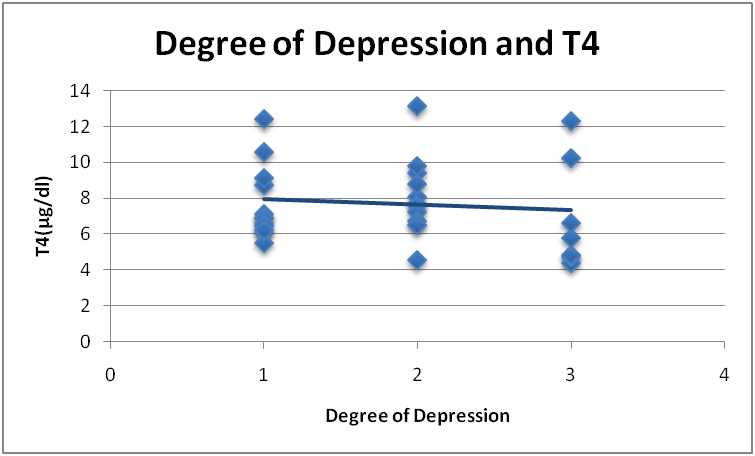
Higher mean T4 was recorded in controls compared to cases and in moderate depression but the difference between the two groups and degree of depression was not statistically significant (P˃0.05).
No significant correlation was found between TSH and cases compared to controls even though higher mean was recorded in depressed cases (P˃0.05).
There was a significant positive correlation between TSH and severe depression in subjects depicted in table 2 (ρ=0.37, P˂0.04*). Significant positive correlation was found between T3,T4 and TSH, showing inverse relation of T3,T4 with TSH shown in [Table 3] and [Figure 1],[Figure 2],[Figure 3] respectively.
| Parameter | Cases | Controls | P value | ||
| Mild | Moderate | Severe | |||
| BMI | 22.91±3.80 | 22.54±2.84 | 23.28± 2.13 | 21.76±2.34 | 0.09 |
| FBS | 84.58 ±8.19 | 86.72 ±6.19 | 85.42 ±8.94 | 83.96 ±8.55 | 0.32 |
| T3 | 107.28 ±15.34 | 102.13 ±24.15 | 93.67 ±34.01 | 103.43±15.50 | 0.89 |
| T4 | 7.70 ±2.07 | 8.12 ±2.21 | 6.97 ±3.08 | 8.11 ± 1.73 | 0.20 |
| TSH | 1.81 ±1.25 | 3.86 ±2.76 | 16.83 ±36.72 | 2.17 ±1.20 | 0.47 |
| Parameters | Degree of depression | |
| Correlation Coefficient | P value | |
| T3 | -0.26 | 0.15 |
| T4 | -0.11 | 0.54 |
| TSH | 0.37 | 0.04* |
| Parameters | Correlation Coefficient | P value |
| T3 Vs T4 | 0.71 | <0.001* |
| T3 Vs TSH | -0.48 | 0.006* |
| T4 Vs TSH | -0.40 | 0.02* |

Discussion
The possibility of a relationship between thyroid gland, brain and behaviour has captured the attention of clinicians and researchers for more than two centuries (Whybrow and Prange, 1981).[9] Even subtle decrease in available thyroid hormone might be expected to produce depressive symptoms directly, on the basis of basic and clinical data on the role of the thyroid axis in mood regulation. In addition, decrease in thyroid function cause decrease in energy, concentration, mood, and drive, which might produce depression on the basis of loss of function, attribution, or other mechanisms.[7]
Our study is aimed to estimate the prevalence of thyroid dysfunction in depressed patients, as it will be beneficial for the treating psychiatrists to be cautious in cases of treatment resistant depression as well.[4]
Correlating with many studies, our study showed increase prevalence of depression in females than their male counterpart, thereby recommending physicians to give special attention to the possibility of female patients with MDD developing overt thyroid dysfunction.[10]
Most of the subjects fell in normal range of BMI, difference in mean BMI between the two groups and degree of depression is not statistically significant but severe depression subjects had higher me an compared to other subtypes, Ann Barrett et al reported that depression is related to obesity, and that increasing severity of depression is also related to obesity, a potential link between the two was also found in the relationship to the amount of physical activity performed.[11]
Comparison of serum FBS between both groups and subtypes of depression is statistically insignificant but cases and severe depression showed higher mean than others. It remains unknown, however, if the dimensional severity of depressive symptoms corresponds with the progressive disruption of glucose homeostasis.[12]
Our study revealed not much significant difference in mean T3 and T4 between both groups and degree of depression but severe depression subjects showed lower mean compared to others. This is concordance with study done by Vinod kumar chopra et al , Linnoila et al., Joffe et al.[9],[13],[14] Significant positive correlation was found between T3,T4 and TSH, showing inverse relation of T3,T4 with TSH. Mildly depressed people usually do not seek medical help while severely depressed people usually go to Emergency for help.[4]
Higher mean TSH is recorded in cases compared to controls and in severe depression but the difference between the two groups and degree of depression is not statistically significant. There is positive correlation between TSH and severity of depression observed in our study which is consistent with study done by Vinod kumar Chopra et al. who suggested that elevated levels of TSH indicate the presence of subclinical hypothyroidism in depressive patients. Since TSH is a sensitive indicator of thyroid function. Ojha SP et al revealed that there was positive correlation between types of depression and thyroid status, Cleare et al[15] found a positive relation between depressive scores and the increase in TSH levels.
Among 30 newly diagnosed depressed subjects 30% showed hypothyroidism in which 22.2% were subclinical hypothyroidism and 77.7% were found to be clinical hypothyroidism.
Increased risk for hypothyroidism in patients with MDD may be related to the disease itself. Many patients with MDD suffer from chronic stress and then experience the fight-or-flight response. Persons with subclinical thyroid disease are often overlooked for treatment.[10]
Understanding the link between depression and thyroid disorders will guide clinicians to appropriately interpret thyroid function tests in depression, in better understanding the pathophysiology of both diseases, and try to identify the subjects who will benefit the most from thyroid supplementation.[5]
Conclusion
The observations made in this study, propose that thyroid hormones play an important role in neuropsychiatric manifestations, such as mood disturbances. The diagnosis of subclinical or clinical hypothyroidism must be considered in every patient with depression. Thus follow-up of these patients with regard to the development of diseases may be beneficial.
Our study was a single hospital based study and consisted of a limited number of newly diagnosed depressed subjects. Further studies with larger number of depressed subjects will be beneficial in elucidating the relationship between thyroid profile and depression, so that TFTs can be considered as an integral part of evaluation of newly depressed subjects.
Ethics approval
The Institutional Ethics Committee approval was obtained from KIMS Institutional Ethics committee, Bangalore
Source of funding
Self funding was done for the study.
Conflict of interest
None
References
- . WHO | depression. World Health Organization. 2011. [Google Scholar]
- P C Dinas, Y Koutedakis, A D Flouris. Effects of exercise and physical activity on depression. Ir J Med Sci 2011. [Google Scholar]
- C Lazarou, M Kapsou. The role of folic acid in prevention and treatment of depression: an overview of existing evidence and implications for practice. Complement Ther Clin Pract 2010. [Google Scholar]
- S P Ojha, S Dhungana, M Chapagain, P Tulachan. Association of thyroid dysfunction with depression in a teaching hospital. J Nepal Health Res Counc 2013. [Google Scholar]
- M P Hage, S T Azar. The Link between Thyroid Function and Depression. J Thyroid Res 2012. [Google Scholar]
- - Burtis, R Edward, David E Ashwood, - Bruns, - Teitz. . Fundamentals of Clinical Chemistry 2008. [Google Scholar]
- M S Gold, A L Pottash, I Extein. Hypothyroidism and depression. Evidence from complete thyroid function evaluation. JAMA 1981. [Google Scholar]
- E H Makela. Hypothyroidism and depression :a therapeutic challenge. Ann Pharmacother 2000. [Google Scholar]
- Ram D Vk. Basal thyroid functions in first episode depressive illness : a controlled study. Indian J Psychiatry 2001. [Google Scholar]
- E L Wu, I C Chien, C H Lin, Y J Chou, P Chou. Increased risk of hypothyroidism and hyperthyroidism in patients with major depressive disorder: a population-based study. J Psychosom Res 2013. [Google Scholar]
- Ann Barrett. Depression and its relationship to physical activity and obesity. The Ohio State University School of Allied Medical Professions. Med Dietetics Program 2012. [Google Scholar]
- L S Kahn, R S Mcintyre, L Rafalson, D E Berdine, C H Fox. Fasting Blood Glucose and Depressive Mood among Patients with Mental Illness in a Medicaid Managed Care Program. Depress Res Treat 2011. [Google Scholar]
- M Linnoila, R Cowdry, B-A Lamberg, T Makinen, D Rubinow. CSF triiodothyronine (rT3) levels in patients with affective disorders. Biol Psychiatry 1983. [Google Scholar]
- R T Joffe. Is the thyroid still important in major depression. J Psychiatry Neurosci 2006. [Google Scholar]
- A J Cleare, A McGregor, S M Chambers, S Dawling, V O'Keane. Thyroxine replacement increases central 5-hydroxytryptamine activity and reduces depressive symptoms in hypothyroidism. Clin Endocrinol 1996. [Google Scholar]
