- Visibility 94 Views
- Downloads 23 Downloads
- Permissions
- DOI 10.18231/j.ijcbr.2022.035
-
CrossMark
- Citation
Hypoproteinemia: An eye of suspicion towards the diagnosis of rapunzel syndrome
- Author Details:
-
Dadasaheb Maindad
-
Gayatri Gawade Maindad *
Abstract
The Rapunzel syndrome is the usually name given to the trichobezoar related condition in which there is extension of tail of trichobezoar from its origin to the distant location. Trichobezoar is the rare clinical entity found usually in the pediatric population and young females with underlying psychiatric condition. There is huge collection of undigested materials like hairs, threads, etc. leading to various clinical complications if not diagnosed and removed on time. Hypoproteinemia is a rare presentation of complication of this Rapunzel syndrome due to protein losing enteropathy. We encountered with the case of hypoproteinemia giving clue to the diagnosis of Rapunzel syndrome.
Case Presentation
Chief complaints
A 16 year-old girl presented with the history of vomiting and abdominal pain in epigastric and umbilical region on and off since 2 months. She was admitted in the hospital for the same and treated symptomatically. She underwent the baseline investigations like abdomen ultrasound, liver function tests (LFT), renal function tests (RFT), hemogram, urine routine and serum amylase, lipase, etc. All the investigations were normal except liver function test and hemogram. The LFT showed that the levels of total protein, albumin and globulins were significantly reduced.
History of present illness
Initially probable diagnosis made was gastritis and so she was started on oral PPI’s, antacids and antiemetics. However the symptoms persisted inspite of above all treatment.
Due to persistent symptoms, the planned gastroscopy was underwent followed by CECT abdomen. Gastroscopy showed large trichobezoar extending from the fundus to the D1-D2 Junction.
History of past illness
There was significant history of hair and thread swallowing unconsciously especially when she was alone. She had not taken any psychiatric treatment for the same.
Personal
There was history of reduced appetite, reduced weight gain and history of pica and hair, thread swallowing.
Family history
There was no history of swallowing hair in family members.
Physical examination
On physical examination, a movable mass was palpable in the left upper quadrant. The epigastric and umbilical area tenderness was there. There was no redness, swelling at the site of mass.
Laboratory investigations
|
S. No. |
Laboratory Parameter |
Result |
|
1 |
Hemoglobin |
7.5 gm% |
|
2 |
Total protein |
4.2 gm/dl |
|
3 |
Albumin |
1.7 gm/dl |
|
4 |
Globulin |
2.3 gm/dl |
|
5 |
A/G ratio |
0.82 |
Imaging examinations
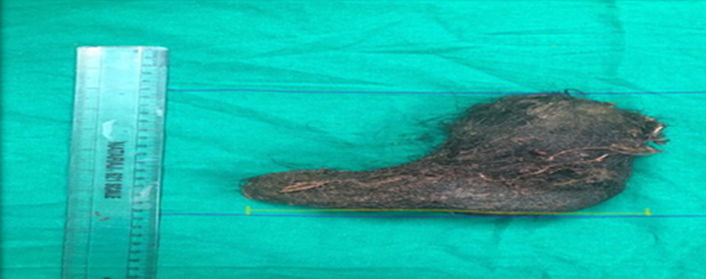
Noninvasive imaging examinations were performed, including plain chest radiography, ultrasound, and contrast enhanced computed tomography (CECT). Plain radiographs showed that the chest was normal. Abdominal ultrasound demonstrated an intragastric hyper echoic mass. CECT scan showed a large heterogeneous, mesh like mass with air sign filling the gastric cavity, measuring approximately 16.5 cm × 9 cm × 4 cm in size ([Figure 1]). Gastroscopy done was showing the large trichobezoar extending from the fundus to D1-D2 junction. That trichobezoar was found to have the undigested hairs and threads. The weight was 50 gm. So based on history, clinical examination and investigations, the final diagnosis was made as the giant gastric trichobezoar leading the Rapunzel syndrome due to trichophagia and trichotillomania.
Treatment
Laparoscopic gastrostomy was performed and the large trichobezoar was removed with the suprapubic incision. Post procedure patient was stable and was referred for psychiatric care after discharge.
Discussion
Bezoars are collections of non digestible matter that usually accumulates in stomach and can extend to small bowel. Different types of bezoars are Phytobezoar (vegetable origin), Trichobezoar (composed mainly of hair), Lactobezoar (concentrated milk formula), Pharmacobezoar (mixed medicine bezoars), and food bolus bezoars. Trichobezoars (concretions of hair) are unusual and are usually found in young psychiatric females, who often deny eating their own hair (trichophagy). It is caused by the pathological ingestion of hair, which remains undigested in the stomach.[1], [2]
Continuous ingestion of hair, over a period of time, can lead to their impaction along with mucus and food material into the stomach. In some cases, the trichobezoar extends through the pylorus into jejunum, ileum or even colon. This condition, called Rapunzel syndrome, was first described by Vaughan et al., in 1968.[3], [2]
Appropriate mastication, proper fluid consumption, and limiting ingestion of high-fiber foods can prevent phytobezoar formation.[4] As one may expect, underlying gastrointestinal pathology, such as previous surgery,[5] adhesions, radiation, gastritis, or dysmotility, can precipitate an obstruction in the setting of bezoar formation.[6]
Treatment options for gastric trichobezoars include medical therapy,[7] electrohydraulic lithotripsy,[8] laser irradiation,[9] extracorporeal shock wave lithotripsy, and endoscopic treatments in which stones are crushed mechanically using a forceps and other instruments and surgical therapy (open abdominal surgery and laparoscopic surgery) to remove the gastric bezoars.[10], [11], [12] There is no or little evidence of simultaneous use of endoscopy and laparoscopy for the trichobezoars removal in the literature making use of principle of LECS (laparoscopy endoscopy cooperative surgery) to overcome the traditional treatment disadvantages suggesting the possible role of this therapy as future treatment modality.[13]
There are a number of complications that can arise from trichobezoars depending on their size, location, and chronicity. Our case presented with severe hypoproteinemia that can be explained due to the chronic severe malabsorption resulting in severe malnutrition.[14], [15], [16] Such cases can present with the anemia that can arise from both iron malabsorption and chronic ulceration indicating the need to keep in mind the critical importance of the nutritional aspect of treatment. If these underlying pathologies left untreated can affect the other developmental milestones and retard the growth of the children.[17]
Conclusion
The differential diagnosis of epigastric tumors in children should consider trichobezoar as one of the entity.
With this case we can conclude that the surgical either endoscopic or laparoscopic removal and nutritional supplementation remains the gold standard treatment of large trichobezoar.
The role of thorough history taking can be highlighted by considering this case
Awareness about the psychiatric counselling in these patients is the need of hour.
The obsessive-compulsive disorders like Trichotillomania and trichophagia may be associated with patients with trichobezoars so should be under psychiatric care to prevent recurrence of the disease.
The routine biochemical parameters like protein estimation gives the clue to the diagnosis of rare entity highlights the importance of critical interpretation of such tests in clinical practice. So, the eye of suspicion should always be kept on.
Source of Funding
None.
Conflict of Interest
The author declares no conflict of interest.
References
- John N, Timothy J, Williams N, Bulstrode C, O’Connell P. Stomach and duodenum. Bailey and Love’s Short Practice of Surgery. 2013. [Google Scholar]
- Dixit A, Raza M, Tiwari R. Gastric Trichobezoar with Rapunzel Syndrome: A Case Report. J Clin Diagn Res. 2016;10(2):10-1. [Google Scholar]
- Vaughan E, Sawyers J, Scott H. The Rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery. 1968;63:339-43. [Google Scholar]
- Mohseni M, Kruse B. An unusual mimic of intermittent bowel obstruction. Am J Case Rep. 2019;20:1920-22. [Google Scholar]
- Ben-Porat T, Elazary R, Goldenshluger A, Sherf-Dagan S, Grinbaum R, Beglaibter N. Phytobezoar: a rare late complication following laparoscopic sleeve gastrectomy surgery. Intl Surg J. 2017;4(5):1803-5. [Google Scholar]
- Mohseni M. An unusual mimic of intermittent bowel obstruction ©. Am J Case Rep. 2019;20:1920-2. [Google Scholar]
- Iwamuro M, Yunoki N, Tomoda J, Nakamura K, Okada H, Yamamoto K. Gastric bezoar treatment by endoscopic fragmentation in combination with Pepsi-Cola® administration. Am J Case Rep. 2015;16:445-8. [Google Scholar]
- Kuo J, Mo L, Tsai C, Chou C, Lin R, Chang K. Nonoperative treatment of gastric bezoars using electrohydraulic lithotripsy. Endoscopy. 1999;31(5):386-8. [Google Scholar]
- Grande G, Manno M, Zulli C, Barbera C, Mangiafico S. An alternative endoscopic treatment for massive gastric bezoars: Ho:YAG laser fragmentation. Endoscopy. 2016;48( Suppl 1). [Google Scholar]
- Kadoya S, Tokuraku M, Harada T. A case of bezoar extracted by laparoscopic surgery. J Jpn Surg Assoc. 2003;64:2741-4. [Google Scholar]
- Ulukent S, Ozgun Y, Şahbaz N. A modified technique for the laparoscopic management of large gastric bezoars. Saudi Med J. 2016;37(9):1022-4. [Google Scholar]
- Zhang R, Yang Z, Fan B. Huge gastric disopyrobezoar: a case report and review of literatures. World J Gastroenterol. 2008;14(1):152-4. [Google Scholar]
- Kurosu T, Tanabe S, Hasegawa R, Yano T, Wada T, Ishido K. A giant trichobezoar extracted by laparoscopic and endoscopic cooperative surgery (LECS). Endosc Int Open. 2018;6(12):1413-6. [Google Scholar]
- Ullah W, Saleem K, Ahmad E, Anwer F. Rapunzel syndrome: a rare cause of hypoproteinaemia and review of literature. BMJ Case Rep. 2016;2016. [Google Scholar] [Crossref]
- Cannalire G, Conti L, Celoni M, Grassi C, Cella A, Bensi G. Rapunzel syndrome: an infrequent cause of severe iron deficiency anemia and abdominal pain presenting to the pediatric emergency department. BMC Pediatr. 2018;18. [Google Scholar]
- Nour I, Alatef M, Megahed A, Yahia A, Wahba Y, Shabaan A. Rapunzel syndrome (gastric trichobezoar), a rare presentation with generalised oedema: case report and review of the literature. Paediatr Int Child Health. 2019;39(1):76-8. [Google Scholar]
- Khanna K, Tandon S, Yadav DK, Khanna V. Rapunzel syndrome: a tail too long to tell!. BMJ Case Rep. 2018;2018:2018-224756. [Google Scholar]
How to Cite This Article
Vancouver
Maindad D, Maindad GG. Hypoproteinemia: An eye of suspicion towards the diagnosis of rapunzel syndrome [Internet]. Int J Clin Biochem Res. 2022 [cited 2025 Sep 22];9(2):182-184. Available from: https://doi.org/10.18231/j.ijcbr.2022.035
APA
Maindad, D., Maindad, G. G. (2022). Hypoproteinemia: An eye of suspicion towards the diagnosis of rapunzel syndrome. Int J Clin Biochem Res, 9(2), 182-184. https://doi.org/10.18231/j.ijcbr.2022.035
MLA
Maindad, Dadasaheb, Maindad, Gayatri Gawade. "Hypoproteinemia: An eye of suspicion towards the diagnosis of rapunzel syndrome." Int J Clin Biochem Res, vol. 9, no. 2, 2022, pp. 182-184. https://doi.org/10.18231/j.ijcbr.2022.035
Chicago
Maindad, D., Maindad, G. G.. "Hypoproteinemia: An eye of suspicion towards the diagnosis of rapunzel syndrome." Int J Clin Biochem Res 9, no. 2 (2022): 182-184. https://doi.org/10.18231/j.ijcbr.2022.035
